Hepatic risk factors associated with chronic kidney disease in nonalcoholic fatty liver disease
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
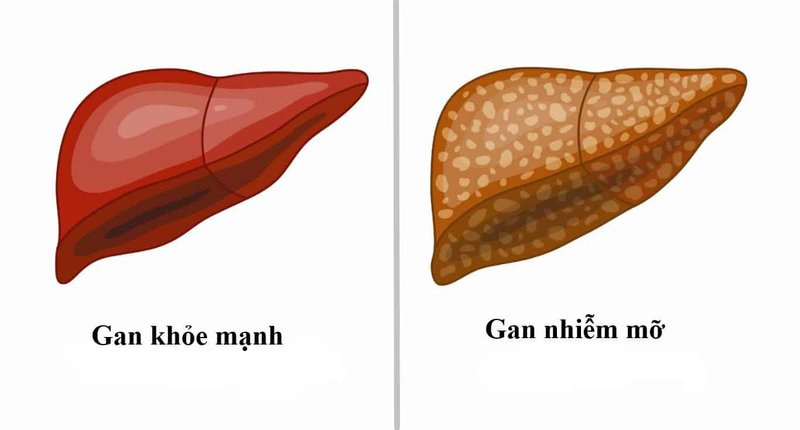
Nonalcoholic fatty liver disease (nonalcoholic fatty liver disease) covers a spectrum of chronic liver diseases, ranging from steatosis on one end to fibrosis and cirrhosis on the other. NAFLD and non-alcoholic steatohepatitis (NASH) are liver manifestations of the metabolic syndrome (MetS), which is the driver of a multitude of comorbidities, such as insulin resistance, heart disease, and heart disease. vascular (CVD), chronic kidney disease (chronic kidney disease), obstruction. obstructive sleep apnea (OSA), as well as an increased risk of malignancy.
1. Liver risk factors
Advanced fibrosis associated with nonalcoholic fatty liver disease :
Patients with advanced fibrosis associated with NAFLD are more likely to develop chronic kidney disease than patients with nonalcoholic fatty liver disease without progressive fibrosis. The risk of albuminuria increases with severity of advanced fibrosis and nonalcoholic fatty liver disease, according to a 2017 study of 1,763 Chinese diabetic patients. After adjustment for common chronic kidney disease risk factors such as diabetes and other metabolic comorbidities, advanced fibrosis but not steatosis was associated with a higher risk of albuminuria (OR: 1 .52; 95% CI: 1.02-2.28; P= 0.039).
In a 2019 study of 594 patients with type 2 diabetes, significant hepatic fibrosis detected by elastography (LSM ≥ 7.0/6.2 kPa) was independently associated with a higher risk of chronic kidney disease (adjusted OR: 3.6, 95% CI: 1.3-10.1; P = 0.01) in addition to CVD and other microvascular complications. Increased liver stiffness as detected by transient elastography is a predictor of chronic kidney disease in patients with non-alcoholic fatty liver disease diagnosed by ultrasound. In a 12-year prospective cohort study, non-obese nonalcoholic fatty liver disease patients had a higher risk of developing chronic kidney disease than obese nonalcoholic fatty liver disease patients.
A recent study noted that the risk of developing chronic kidney disease was higher in metabolically unhealthy non-alcoholic nonalcoholic fatty liver disease patients compared with their counterparts with A healthy metabolic state is defined by the lack of metabolic risk factors (ie, diabetes mellitus, low high-density lipoprotein, hypertriglyceridemia, arterial hypertension).
Pathophysiology: Chronic kidney disease secondary to fatty liver is thought to be caused by systemic low-grade inflammation, possibly related to the regulation of the nuclear factor-κB (NF-κB) pathway. As discussed earlier, there is concrete evidence that patients with advanced fibrosis associated with nonalcoholic steatohepatitis have an increased incidence of chronic kidney disease. The progression of nonalcoholic steatohepatitis may be partly mediated by the altered renin-angiotensin-aldosterone system by chronic kidney disease which has also been suggested as a mechanism for the progression of liver disease. non-alcoholic steatosis. Although direct pathogenic associations between nonalcoholic fatty liver disease and chronic kidney disease appear to be confounded by common metabolic comorbidities, novel mechanisms have been described.
Insulin resistance: Fat gain leads to increased free fatty acids and proinflammatory cytokine release that induce systemic insulin resistance (IR), which is an established mediator of nonalcoholic fatty liver disease. IR is further exacerbated by the progression of non-alcoholic fatty liver disease, leading to atherogenic dyslipidemia and further release of inflammatory cytokines leading to chronic kidney disease as shown in tissues animal figure. Prostatitis occurs through the NF-κB and Jun-N-terminal kinase (JNK) pathways; Activation of fat-specific JNK pathways has been shown to induce insulin resistance. When NAFLD progresses to NAFLD, the inflammatory component predominates neutrophils and may cause systemic endothelial dysfunction. Notably, IR resulted in increased production of very low density lipoproteins and endoplasmic reticulum stress, both of which can induce glomerular podocyte injury. The latter two mechanisms are involved in proteinuria and the subsequent rapid proliferation of chronic kidney disease.

Two established mechanisms between nonalcoholic fatty liver disease and the development of chronic kidney disease are fat gain and insulin resistance. NF-κB: Nuclear Factor-κB; JNK: Jun kinase N-terminal; ROS: Reactive Oxygen Types; NO: Nitric oxide; CRP: C-reactive protein; IL-6: Interleukin-6; VLDL: Very low density lipoprotein; TNF-α: Tumor necrosis factor alpha; CKD: Chronic kidney disease
Ectopic lipid accumulation:
In animal models, a high-fat/fructose diet resulted in increased urinary albumin excretion, increased transaminases, and increased incidence of liver tumors compared with a digestible diet. standard. Microscopically, lipid deposition leads to increased liver disease, suggesting that cellular lipid accumulation may link nonalcoholic fatty liver disease with chronic kidney disease. With fenofibrate treatment, slower cellular lipid accumulation has been observed concomitantly with slower progression of liver and kidney disease.
Wnt signaling abnormalities: Changes in cellular pathways important for homeostasis play an important role in the development of chronic kidney disease in patients with non-alcoholic fatty liver disease. Alcohol . Specifically, abnormalities in the Wnt signaling pathway (named as a combination of the wingless Drosophila gene and the integrated, vertebrate homolog) are associated with lipid accumulation, chronic inflammation, and chronic inflammation. and fibrosis in the development of both nonalcoholic fatty liver disease and chronic kidney disease. Sterol regulatory factor binding proteins: Sterol regulatory factor binding proteins are activated in a nutrient-rich state (i.e. anabolic) leading to insulin signaling and increased endoplasmic reticulum stress, which can cause lipogenesis and hepatitis. These changes induce the progression of other metabolic phenomena such as chronic kidney disease and MetS.
Fructose consumption and uric acid accumulation: Fructose intake is associated with hepato-renal injury through uric acid accumulation by altering the gut microbiome. Patients with normal body mass index (BMI) and high serum uric acid levels (>10 mg/dL) have an increased incidence of MetS when compared with patients with serum uric acid <6 mg/dL. dL, as demonstrated by other studies. An increase in serum uric acid levels is also associated with an increased incidence of nonalcoholic fatty liver disease. In patients with nonalcoholic fatty liver disease, elevated uric acid levels are known to be causative in the progression of chronic kidney disease. These studies suggest that MetS, nonalcoholic fatty liver disease, and chronic kidney disease are connected through increased serum uric acid levels.

Fructose consumption and uric acid accumulation play an important role in patients with nonalcoholic fatty liver disease who develop chronic kidney disease. TMAO: Trimethylamine N-oxide; SCFAs: Short-chain fatty acids; RAAS: renin-angiotensin-aldosterone system; PNPLA3: 3-domain protein containing phospholipase like Patatin; CKD : Chronic kidney disease; NF-κB: Nuclear Factor-κB.
Uric acid stimulates fructokinase, which sensitizes hepatocytes to metabolize fructose, which then leads to fat deposition in the liver, thus explaining the link between hyperuricemia and nonalcoholic fatty liver disease. Elevated uric acid levels in animal models lead to glomerular hypertension and interstitial fibrosis, two processes that preclude the development of chronic kidney disease. Reduced uric clearance in patients with chronic kidney disease may exacerbate this condition. Interestingly, xanthine oxidase inhibitors are currently being tested in chronic kidney disease patients to monitor disease progression in chronic kidney disease -FIX.
Disorders of gut microbiota: Changes in the gut microbiota play a role in the pathogenesis of nonalcoholic fatty liver disease and chronic kidney disease. Dietary conditions such as increased fructose intake and vitamin D deficiency are thought to cause dysbiosis, which may directly lead to low-grade inflammation that causes the development of nonalcoholic fatty liver disease and chronic kidney disease. Dysbiosis and subsequent microbial fermentation lead to increased production of the uremic toxins indoxyl sulfate and p-cresyl sulfate, which is directly correlated with the progression of chronic kidney disease. The hepatic cytochrome P450 enzymes are directly regulated by these urea toxins derived from changes in the metabolism of the gut microbiota, thus the gut-liver-kidney axis.
Animal models also show the gut microbiota's ability to convert choline to trimethylamine N-oxide (TMAO), which is considered both nephrotoxic and hepatotoxic. In a 2015 study comparing TMAO levels in patients with chronic kidney disease (n = 521) with healthy patients (n = 3166), mean TMAO levels were significantly higher in patients with chronic kidney disease. (P < 0.001). Similarly, a 2019 case-control study comparing patients with nonalcoholic fatty liver disease (n = 34) with those without (n = 14) found that TMAO played a role in aggravating fatty liver disease. liver. Finally, some species in the gut microbiota produce short-chain fatty acids (SCFAs) such as butyrate, acetate and propionate and diffuse across the intestinal mucosa, which can disrupt the integrity of the intestinal barrier. In the blood, SCFAs can cause systemic inflammation, a common causative link between nonalcoholic fatty liver disease and chronic kidney disease.
Genetic link between non-alcoholic fatty liver disease and chronic kidney disease : Two gene variants associated with both chronic kidney disease and non-alcoholic fatty liver disease are the G allele of a gene containing a patatin-like phospholipase-containing domain (PNPLA3) and the T allele of the transmembrane 6-membered superfamily gene 2 (TM6SF2). The G allele in the rs738409 polymorphism of the PNPLA3 gene has been shown to play an important role in the progression of nonalcoholic steatohepatitis [72, 73]. Patients with the G allele have also been shown to have a lower eGFR, an increased rate of microalbuminuria, and an increased incidence of chronic kidney disease, regardless of nonalcoholic fatty liver disease status/nonalcoholic steatohepatitis. . The patient populations found to be at highest risk for chronic kidney disease and non-alcoholic fatty liver disease in a 2015 study were patients with the G allele of PNPLA3 ; Furthermore, these patients were not obese, which is an important risk factor for chronic kidney disease. Another study showed that Chinese patients with normal alanine aminotransferase levels carrying the rs738409 polymorphism in the PNPLA3 gene had an increased risk of early glomerular and tubular damage, which may explain why these patients develop chronic kidney disease even in the absence of well-known risk factors, like obesity or diabetes.
In postmenopausal women with type 2 diabetes, having the G/G allele leads to a higher incidence of chronic kidney disease, regardless of nonalcoholic fatty liver disease status, further supporting the argument that this polymorphism could be an independent predictor of chronic kidney disease. Patients found to have the G/G allele in the rs738409 polymorphism should be closely monitored for the development of nonalcoholic fatty liver disease as well as renal dysfunction, even in normal-weight patients. often. On the other hand, the rs58542926 polymorphism on the TM6SF2 gene, also known as the T allele of the TMS6F2 gene, is associated with the development of non-alcoholic fatty liver disease but is also associated with higher eGFR and albuminuria rates lower trace. Thus, this specific polymorphism in TM6SF2 may be nephroprotective in patients with nonalcoholic fatty liver disease.
Để đặt lịch khám tại viện, Quý khách vui lòng bấm số HOTLINE hoặc đặt lịch trực tiếp TẠI ĐÂY. Tải và đặt lịch khám tự động trên ứng dụng MyVinmec để quản lý, theo dõi lịch và đặt hẹn mọi lúc mọi nơi ngay trên ứng dụng.
Bài viết này được viết cho người đọc tại Sài Gòn, Hà Nội, Hồ Chí Minh, Phú Quốc, Nha Trang, Hạ Long, Hải Phòng, Đà Nẵng.