Why do thin people also get non-alcoholic fatty liver disease?
Post by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
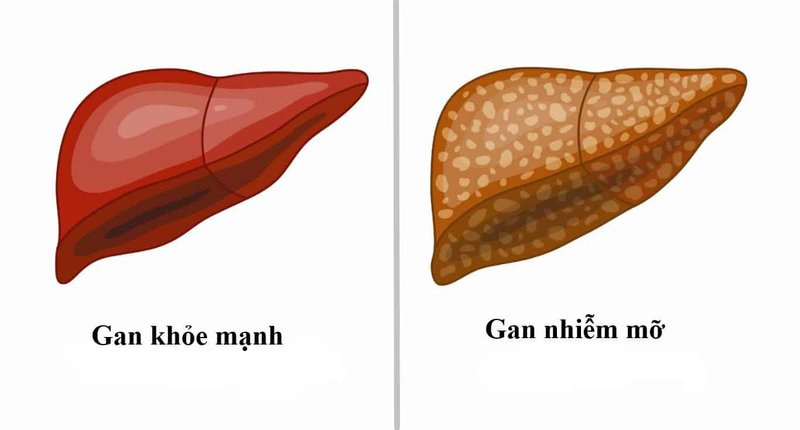
Nonalcoholic fatty liver disease (NAFLD) has been recognized as a major cause of chronic liver disease in the industrialized world. The incidence of nonalcoholic fatty liver disease is not only increased in patients with type 2 diabetes, metabolic syndrome, and obesity, but is also associated with more severe forms of the disease, a significant proportion of subjects developing NAFLD despite having a relatively normal body mass index (BMI), a condition known as non-obesity or non-alcoholic fatty liver disease in lean people.
1. Pathogenesis – why do thin people still get nonalcoholic fatty liver disease?
Thin people still suffer from non-alcoholic fatty liver disease, several causes of this problem have been implicated, such as high fructose intake, protein malnutrition (Kwashiorkor) as well as use of steatogenic drugs (amiodarone) , tamoxifen, methotrexate, prednisolone, etc.) and genetic predisposition.
Romeo et al highlighted the involvement of the single nucleotide polymorphism rs738409 in the protein containing the patatin-like phospholipase 3 domain (PNPLA 3) gene initiating and progressing NAFLD. However, numerous other gene variants have also been implicated in increased susceptibility to NAFLD/NASH and progression to liver fibrosis and even HCC, such as transmembrane superfamily 2 member 6 (TM6SF2) , the glucokinase regulatory gene (GCKR) and the membrane-associated O-acyltransferase domain containing 7 genes (MBOAT7). In addition, a variant of the interferon-λ3 (IFN-λ3) gene was associated with increased inflammation and liver fibrosis in NAFLD patients, while the rs72613567 polymorphism in the hydroxysteroid 17-beta dehydrogenase 13 gene ( HSD17B13) has recently been shown to reduce the risk of liver fibrosis, NASH, and HCC. Notably, both dietary composition and socioeconomic factors were correlated with NAFLD development. Adherence to the Mediterranean diet has been shown to improve insulin sensitivity in the liver and reduce fat accumulation in the liver while the Western diet, which mainly consists of high amounts of fructose and saturated fat, has involved in the development of NAFLD. Furthermore, prolonged periods of sitting, often associated with high calorie intake and an unhealthy diet, and reduced physical activity are independent risk factors for NAFLD, even in lean individuals.

Nếu người gầy ăn nhiều fructose vẫn có thể bị bệnh gan nhiễm mỡ không do rượu
2. Current data
Current data on the worldwide prevalence of non-obese non-alcoholic fatty liver disease/nonalcoholic fatty liver disease in lean individuals are characterized by wide variability. In a recent systematic review including 84 studies involving 10530308 individuals, Ye et al demonstrated that in the general population, the prevalence of lean and non-obese NAFLD was 5.1% and 12, respectively. first%. In addition, the overall prevalence of NAFLD in the general lean population was 10.6%, while the prevalence of NAFLD in the non-obese population was 18.3%. Interestingly, the prevalence of non-obese NAFLD in the total NAFLD population was highest in Europe (51.3%) and lowest in East Asia (37.8%). Notably, NAFLD patients were classified according to World Health Organization (WHO) and Asia Pacific recommendations as overweight and underweight when their BMI was 25 to 30 kg/m2 and << 25 kg/m 2, in non-Asian subjects, and 23 kg/m 2 to 27.5 kg/m 2 and < 23 kg/m 2, respectively, in the Asian population. However, it is well established that individuals with similar BMIs may have varying degrees of visceral obesity, which is strongly associated with the development of NAFLD. Waist circumference is considered to be a more accurate marker of visceral obesity than BMI, but was not available in the majority of related studies. This editorial will discuss the metabolic profile, prognosis, and associated clinical outcomes, as well as the management of non-obese or lean patients with NAFLD.
3. Clinical impact of non-obese/thin non-alcoholic fatty liver disease
Younossi et al in a study conducted in the United States reported that lean NAFLD patients (BMI <25 kg/m2) compared with healthy lean individuals had a higher prevalence of insulin resistance (IR), diabetes type 2, hypercholesterolemia and higher blood pressure, i.e. components of the metabolic syndrome. In the NHANES III cross-sectional study, Golabi et al. reported that patients with lean NAFLD (BMI <25 kg/m2), had a higher all-cause risk [Hazard ratio (HR): 1.54 ] and related cardiovascular mortality (HR: 2.38) compared with non-NAFLD lean subjects after adjusting for potential confounding variables. Interestingly, in another study from the United States, Zou et al showed that in the non-obese population (BMI <30 kg/m 2 for non-Asian and <27 kg/m 2 with Asians), NAFLD patients had higher blood pressure, fasting blood glucose (fasting blood sugar), insulin, total cholesterol (total cholesterol), low-density lipoprotein cholesterol (LDL-C), and triglyceride levels and Higher Homeostasis Model Assessment for insulin resistance (HOMA-IR), a marker of IR, compared with subjects without NAFLD. In addition, the group had previously experienced increased cardiovascular, cardiovascular, and cancer-related mortality during the 15-year follow-up period, but these findings were not confirmed in the multivariate analysis

Bệnh nhân gan nhiễm mỡ không do rượu ở ngươi gầy có nguy cơ về biến cố tim mạch hơn bình thường
Thin patients with NAFLD had higher blood pressure, increased fasting blood glucose, and serum triglycerides In a post hoc analysis of Japanese subjects, Yoshitaka et al. reported that thin patients (BMI << 23 kg/m2) with NAFLD had higher blood pressure, increased fasting blood glucose, and serum triglyceride levels, as well as a higher risk (HR: 10.4) for cardiovascular events than for those with NAFLD. in subjects without lean NAFLD, independent of potential confounders. In a retrospective cohort study of 4629 lean Japanese (BMI <23 kg/m2) enrolled in a routine wellness program, Fukuda et al. showed that NAFLD patients had an increased incidence of the disease. type 2 diabetes was 3 times higher than in subjects without NAFLD. Regarding the non-obese subjects, Nishioji et al found that non-obese Japanese NAFLD patients (BMI <25 kg/m2) had a higher prevalence of metabolic syndrome components compared with those who were not obese. strong. Both retrospective and prospective studies from Korea also showed that non-obese NAFLD patients had a higher risk of developing type 2 diabetes than non-obese NAFLD subjects, independent of other factors. other risk factors. Furthermore, Sung et al in a large group of non-obese Koreans (BMI <27 kg/m2), reported that non-obese NAFLD patients had a higher estimated cardiovascular risk based on risk scores. Framingham compared with healthy controls. , while in another Korean cross-sectional study, non-obese (BMI <25 kg/m2) subjects without NAFLD had a better metabolic profile than non-obese patients with NAFLD. Accordingly, Kwon et al., in another retrospective study from Korea, showed that non-obese NAFLD patients (BMI <25 kg/m2) had a higher prevalence of metabolic syndrome components compared with NAFLD patients. with non-obese and yes control groups.
Để đặt lịch khám tại viện, Quý khách vui lòng bấm số HOTLINE hoặc đặt lịch trực tiếp TẠI ĐÂY. Tải và đặt lịch khám tự động trên ứng dụng MyVinmec để quản lý, theo dõi lịch và đặt hẹn mọi lúc mọi nơi ngay trên ứng dụng.
Bài viết này được viết cho người đọc tại Sài Gòn, Hà Nội, Hồ Chí Minh, Phú Quốc, Nha Trang, Hạ Long, Hải Phòng, Đà Nẵng.