Diagnosis and treatment of asthma in children under 5 years of age
Asthma is a common condition in children. Children with asthma under the age of 5 are often difficult to diagnose and treat because the cause is difficult to identify and the symptoms are atypical.
1. Difficulty in diagnosis and treatment of asthma in children
Asthma is a chronic inflammatory condition of the airways with conditions such as constriction, edema, increased sputum secretion, ... causing obstruction, restriction of breathing airflow, and signs such as wheezing, heaviness in the chest. , shortness of breath, recurrent cough. Asthma usually occurs at night and early in the morning and may resolve on its own or with medication.
The prevalence of asthma in adults is 5% and in children it is 10%. Asthma in children under 5 years old is often difficult to diagnose and treat for the following reasons:
Causes of asthma in children are diverse and difficult to determine. In particular, asthma in children under 1 year of age is often confused with bronchiolitis. The differential diagnosis is also quite difficult; Asthma symptoms in young children are atypical and difficult to identify; Laboratory tests, especially respiratory function, are difficult to perform because young children do not know how to cooperate with doctors; Adherence to treatment and implementation of asthma control methods in children under 5 years of age face many difficulties.

Hen gây tắc nghẽn, hạn chế luồng khí thở gây khó thở ở trẻ
2. Diagnosis of asthma in children under 5 years old
In order to make an accurate diagnosis to determine whether a child has bronchial asthma or not, it is necessary to rely on the history, clinical and laboratory symptoms and consider the differential diagnosis with other diseases. Specifically:
2.1 Clinical symptoms
Characteristic symptoms: Children with wheezing accompanied by 1 of the symptoms such as cough, difficulty breathing; Any signs such as: Frequent recurrence of symptoms, worse at night and early morning; symptoms occur with exertion, crying, laughing, exposure to tobacco smoke, pets, cold air; a history of allergies (eczema, allergic rhinitis); occurs in the absence of a respiratory infection; family history of asthma or allergies; crackles or snoring on auscultation; response to asthma treatments; The symptoms of wheezing in children need to be properly identified by a doctor because a child's parents may confuse wheezing with other abnormal breathing sounds.
2.2 Subclinical diagnosis
There is no definitive diagnostic test for asthma in children under 5 years of age. The pediatric patient may have the following tests and the doctor will diagnose the disease based on the results obtained:
Chest X-ray : Routine examination not recommended. Chest X-ray is indicated in cases of severe asthma or clinical signs suggestive of other diagnoses; Skin prick test (specific IgE quantification): Used to assess sensitization to allergens. A positive test result increases the likelihood of a diagnosis of childhood asthma. However, a negative skin prick test does not rule out asthma; Oscillometric oscilloscope (IOS): A specialized method of measuring airway resistance, helping doctors assess airflow limitation of pediatric patients; Measurement of FeNO: Helps assess airway inflammation but is not recommended for routine use.
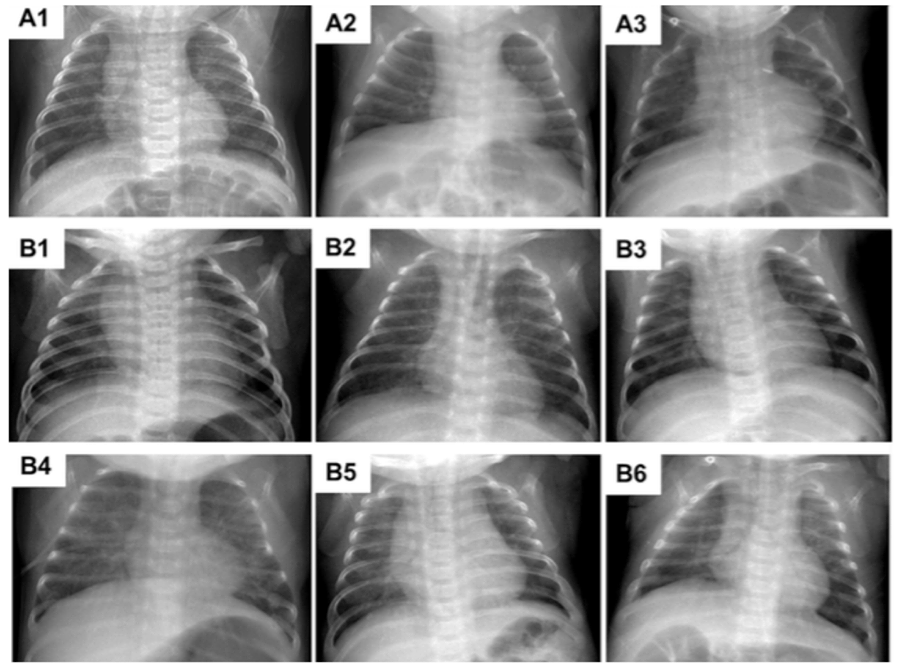
Chụp X-quang ngực giúp chẩn đoán cận lâm sàng, nhưng không được khuyến cáo
2.3 Definitive diagnosis of asthma
Diagnose children with bronchial asthma if they meet the following 5 criteria:
Wheezing, recurrent cough; Have airway obstruction syndrome with clinical manifestations of crackles, snoring; Have a personal or family history of allergies, asthma triggers; Responds to bronchodilators or responds to a 4- to 8-week trial, worsens on discontinuation of therapy; Other causes of wheezing have been ruled out.
Wheezing, recurrent cough; Have airway obstruction syndrome with clinical manifestations of crackles, snoring; Have a personal or family history of allergies, asthma triggers; Responds to bronchodilators or responds to a 4- to 8-week trial, worsens on discontinuation of therapy; Other causes of wheezing have been ruled out.
2.4 Differential diagnosis of asthma with other diseases
Symptoms of wheezing are not only specific to asthma but also a manifestation of many other diseases. Therefore, children with wheezing suspected of having asthma should perform a bronchodilator test (nebulizing salbutamol 2.5mg/time, spraying 2-3 times in a row 20 minutes apart). If the child does not respond or respond poorly after 1 hour, it should be considered with differential diagnoses such as:
Rhinitis: There is an unusual breathing sound coming from the nasopharynx, when examining the nasopharynx, discharge is found in the nose and throat. posterior nose, accompanied by foul odor, pulmonary examination is completely normal; Bronchiolitis: Seen in children under 24 months of age, with first-time wheezing, symptoms of upper respiratory tract virus infection and poor response to bronchodilators; Airway foreign body: A condition that occurs suddenly, the child has symptoms of dyspnea, stridor, cough, history of invasive syndrome, chest X-ray shows a picture of localized air stasis in one lung. , when bronchoscopy detects foreign bodies; Bronchial compression due to mediastinal tumors, bronchial cysts, enlarged lymph nodes: Children have symptoms of wheezing, coughing, prolonged shortness of breath, unresponsive to bronchodilators. Diagnosis of this condition is based on chest x-ray, chest CT scan will show a tumor compressing the airway; Eosinophilic pulmonary infiltrates: Clinically similar to asthma, but caused by parasites, roundworms, drugs or other allergens. The condition progresses well and may resolve on its own; Anatomical malformations (congenital tracheal loop or stenosis), functional abnormalities (vocal cord dysfunction, tracheobronchial dyskinesia): Children present with early wheezing (before 6 months of age): year old). To confirm the diagnosis, it is necessary to combine clinical symptoms and tests such as bronchoscopy and computed tomography; Gastroesophageal reflux or tracheoesophageal fistula, recurrent aspiration syndrome: The patient has a history of regurgitation or recurrent respiratory infections. Definitive diagnosis of this pathology by esophageal pH measurement, esophagoscopy and contrast esophagography; Congenital immunodeficiency: The child's manifestations are recurrent respiratory infections, unresponsive to conventional antibiotic treatment, family history of siblings with congenital immunodeficiency. born.

Bệnh hen thường dễ nhầm lẫn với bệnh trào ngược dạ dày thực quản
3. Treatment of asthma in children
3.1 Treatment of acute asthma attacks
Home treatment
Initial treatment: 2 sprays of salbutamol 200mcg, can be repeated every 20 minutes if necessary; Take the child to medical facilities as soon as possible; Take your child to a medical facility right away if he or she has any of these symptoms, including: Difficulty breathing; Symptoms do not improve after 6 sprays of bronchodilator in 2 hours; Parents or caregivers who are unable to manage an acute asthma attack at home. Hospital treatment
For mild asthma: Outpatient treatment using nebulizer salbutamol 2.5 mg/time or MDI salbutamol with spacer (2 - 4 puffs/time) every 20 minutes, 3 times as needed and reassess after each nebulization; Evaluation after 1 hour of treatment; Children respond well to treatment if the wheezing is gone, there is no difficulty in breathing and the SaO2 is 95% or higher. Children respond to treatment incompletely if they still have rales, still have difficulty breathing and SaO2 reaches 92-95%. Children do not respond to treatment if there are crackles, shortness of breath, chest indrawing and SaO2 less than 92%; If the child responds well, continue outpatient treatment with salbutamol MDI every 3 to 4 hours for 24 to 48 hours and schedule a follow-up visit. If the child does not respond completely, give the child nebulized salbutamol and nebulizer Ipratropium 250mcg/time or give the child oral prednisone early if not responding to 1 time nebulized salbutamol. If the child does not respond to treatment, the child will be hospitalized. Treat by nebulizing salbutamol and nebulizing Ipratropium 3 times if necessary. Give the child to take Prednisolone after 3 times without relief, then treat like a severe asthma attack;

Cho trẻ uống Prednisolon sau 3 lần không giảm thì xử trí như cơn hen nặng
For moderate asthma: Outpatient treatment using nebulizer salbutamol 2.5 mg/time or MDI salbutamol with spacer (6 - 8 puffs/time) every 20 minutes, 3 times if needed and re-evaluate after each nebulization; From the step of “assessment after 1 hour of treatment” follow the same steps as in the case of a mild asthma attack; For severe asthma: Requires emergency admission with oxygen mask measures, salbutamol and Ipratropium nebulizers every 20 minutes - done 3 times (reassess after each inhaler), additional hydrocortisone or Intravenous methylprednisolone; Evaluation after 1 hour of treatment; If the child does not respond completely, then resuscitation, nebulize salbutamol every hour; nebulized Ipratropium every 2 - 4 hours, possibly using high-dose ICS, hydrocortisone or intravenous methylprednisolone; Intravenous magnesium sulfate for children over 1 year old; intravenous infusion of Aminophyllin; intravenous infusion of salbutamol, intubation and mechanical ventilation; If the child responds well (manifesting no dyspnea, SaO2 95% or more), continue nebulizing salbutamol, possibly nebulizing Ipratropium every 4-6 hours for 24 hours; intravenous hydrocortisone or intravenous methylprednisolone; Outpatient treatment: MDI salbutamol every 3 - 4 hours for 24 - 48 hours, take Prednisolone 3 days, follow-up appointment; With a critical asthma attack: Need to go to the emergency room with measures to breathe oxygen through a mask; use adrenaline subcutaneously every 20 minutes - do 3 times; nebulization of salbutamol in combination with Ipratropium every 20 minutes - 3 times (reassess after each nebulizer); additional use of hydrocortisone or intravenous methylprednisolone; From the "assess after 1 hour of treatment" step, proceed in the same way as in the case of a severe asthma attack. Note: The drugs are used in appropriate doses according to the correct treatment regimen.

Khi trẻ xuất hiện những cơ hen nặng cần nhập viện cấp cứu với các biện pháp thở oxy qua mặt nạ
Medicines and measures not to be used in acute asthma:
Antibiotics: Only used when there is evidence of infection; Infusion: Only perform when there are signs of dehydration (when infusion should be careful, avoid overloading); Sedatives, drugs to loosen secretions, cough syrups containing dextromethorphan, drugs that reduce secretions of the antihistamine group, physical therapy.
3.2 Maintenance treatment
The goals of asthma treatment in children are good control of symptoms, maintenance of normal activities of the child, reduction of the risk of future deterioration (reducing the risk of acute asthma attacks, ensuring functional breathing and lung development), minimizing the side effects of the drug.
Subjects on maintenance therapy
Children with asthma symptoms, uncontrolled, wheezing episodes (3 or more episodes in 1 season); Children with severe episodes of viral wheezing but with low frequency (1-2 episodes/season); Children are being monitored regularly, need to use SABA (short-acting beta 2 agonist) inhaled regularly (1 - 2 times/week or more); The child was hospitalized for a severe asthma attack. Select maintenance therapy
Viral-onset intermittent wheezing: Use Montelukast (LTRA); Multifactorial wheezing: Inhaled corticosteroids (ICS). Maintenance treatment according to the severity of asthma
Intermittent asthma: Use inhaled SABA as needed or LTRA (leukotriene receptor antagonist); Mild persistent asthma: Use low dose ICS, can use LTRA instead; Moderately persistent asthma: Use moderate dose ICS or low dose ICS in combination with LTRA; Severe persistent asthma: Use high-dose ICS or moderate-dose ICS in combination with LTRA. In the case of children under 5 years of age with intermittent asthma, LTRA can be used during the onset of symptoms of upper respiratory tract virus infection, maintained for 7-21 days.

Tthuốc được chỉ định điều trị duy trì hen ở trẻ, tuy nhiên cần dựa vào mức độ nặng của hen
Treatment according to the level of asthma symptom control
The choice of medication will depend on the degree of asthma control. This helps control symptoms, reduces the risk of an asthma attack and the side effects of medications later on. There are 4 steps of treatment with different levels of asthma symptom control and the use of drugs with drugs and dosages will be decided by the doctor on a case-by-case basis according to the correct treatment regimen.
Assess response and adjust asthma treatment plan in young children
Prior treatment may result in good control, partial control, or no control of symptoms. Depending on each specific case, the doctor will evaluate to adjust the appropriate asthma treatment plan for the child.
Re-examination
Re-examination of the child within 1 week after each acute asthma attack. The frequency of follow-up visits will depend on the degree of asthma control, response to treatment, and the parents' ability to self-manage. The appropriate time for re-examination is 1 - 3 months after starting treatment, then every 3 - 6 months for a follow-up examination; When re-examination, it is necessary to assess the level of asthma control, risk factors, drug side effects, adherence to treatment, and monitor the child's height at least once a year; For children whose spirometry or pulse oscillation is measured, it is necessary to measure every 3 months to decide whether to increase or decrease the treatment step. Discontinue asthma treatment in children under 5 years of age if the child is symptom-free within 6-12 months, is on the lowest step of treatment, and has no other risk factors. In particular, do not stop treatment in the season when the child has a respiratory infection, a high pollen season or when the child is traveling. In case of discontinuing maintenance treatment, it is advisable to re-examine after 3 - 6 weeks to check, if symptoms appear, treatment should be resumed.
To prevent asthma in children under 5 years old, it is necessary to pay attention to breastfeeding from birth, limit the use of broad-spectrum antibiotics in the first year of life, avoid exposure to tobacco smoke, kitchen smoke, pollen, house dust, healthy weight control for babies, avoid overweight, obesity,...
To register for an examination at Vinmec International General Hospital, you can contact the Health System Hotline Vinmec clinics nationwide, or register online HERE.
Bài viết này được viết cho người đọc tại Sài Gòn, Hà Nội, Hồ Chí Minh, Phú Quốc, Nha Trang, Hạ Long, Hải Phòng, Đà Nẵng.






