This article is consulted by Specialist Doctor I Võ Thị Thùy Trang - a gastrointestinal endoscopy specialist at the General Internal Medicine - Outpatient Department, Vinmec Da Nang International Hospital, with many years of experience in the field of gastrointestinal endoscopy.
The pancreas is an important organ that secretes enzymes essential for digestion. The presence of pancreatic stones not only obstructs the excretory ducts of these enzymes but also causes pancreatitis. This is a dangerous complication that can lead to multiple organ failure or, in some cases, be life-threatening if not detected early and treated promptly.
1. What are pancreatic stones?
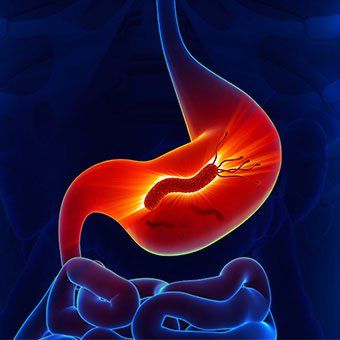
Pancreatic stones form and develop from calcium deposits within the pancreas. As the size of pancreatic stones increases, they can block the secretion of digestive enzymes from the pancreas into the small intestine, leading to stasis and causing pancreatitis. Pancreatic stones are a primary cause in individuals with chronic pancreatitis, a condition often associated with excessive alcohol consumption over a long period.
Additionally, 20 to 30% of patients with chronic pancreatitis due to causes other than pancreatic stones may also develop small pancreatic stones. When pancreatic stones obstruct the pancreatic duct, the pancreas cannot release digestive enzymes into the small intestine, triggering an acute pancreatitis episode.
Moreover, pancreatic function deteriorates in such cases; the pancreas loses its ability to secrete hormones that regulate blood sugar levels, leading to secondary diabetes in patients with chronic pancreatitis.
2. Are pancreatic stones dangerous?
If pancreatic stones are small, they may remain silent in place without causing any symptoms. Conversely, when pancreatic stones grow larger, especially with the impact of chronic inflammatory factors during acute episodes, they can block the pancreatic duct, leading to acute pancreatitis. This vicious cycle results in both chronic pancreatitis and recurrent acute episodes.
The prolonged presence of this condition reduces pancreatic function, leading to poor nutrient absorption, and malnutrition. In severe cases, it can become life-threatening due to multiple organ failure or circulatory collapse during acute pancreatitis attacks.
Pancreatic inflammation leads to pancreatitis. Clinically, pancreatitis may manifest as acute pancreatitis (sudden onset lasting a few days) or chronic pancreatitis (progressing over several years). Depending on individual conditions and severity, mild pancreatitis cases may resolve without treatment, while severe cases can result in life-threatening complications.
3. What are the symptoms of pancreatitis?
The signs and symptoms of pancreatitis can vary depending on whether it is acute or chronic, the classification of inflammation, and the extent of affected pancreatic tissue.
Symptoms of acute pancreatitis include:
- Upper abdominal pain
- Pain radiating to the back
- Increased abdominal pain after eating
- Fever
- Rapid heartbeat
- Nausea
- Vomiting
- Abdominal wall rigidity
Symptoms of chronic pancreatitis include:
- Upper abdominal pain
- Persistent, dull pain
- Weight loss, emaciation
- Fatty stools

4. What are the possible complications of pancreatic stones?
Small pancreatic stones themselves are completely benign and do not affect health. However, when pancreatic stones cause pancreatitis, they become dangerous due to the potential for serious complications, including:
- Pancreatic pseudocyst: Acute pancreatitis can lead to the accumulation of pancreatic fluids and damaged pancreatic tissue, forming a cyst-like sac in the remaining part of the pancreas. A large pseudocyst that ruptures can cause severe complications such as massive internal bleeding and peritonitis.
- Infection: Acute pancreatitis can compromise the pancreas' self-defense, making it susceptible to bacterial invasion and infection. Pancreatic infections are severe inflammatory conditions requiring emergency treatment, including surgery to remove infected tissue, localize the inflammation, and clean the abdominal cavity.
- Kidney failure: Acute pancreatitis can lead to kidney failure. While dialysis can help if kidney failure is severe, without timely intervention, the patient's condition can become critical.
- Respiratory failure: Acute pancreatitis can trigger chemical changes in the body that affect lung function, dangerously lowering blood oxygen levels.
- Secondary diabetes: Damage to insulin-producing cells in the pancreas due to chronic pancreatitis can lead to diabetes due to a lack of insulin secretion, resulting in excessively high blood sugar levels.
- Malnutrition: Both acute and chronic pancreatitis can impair the pancreas’ ability to produce essential enzymes for digesting and absorbing nutrients from food, leading to malnutrition, diarrhea, and weight loss, even if the patient maintains a normal diet.
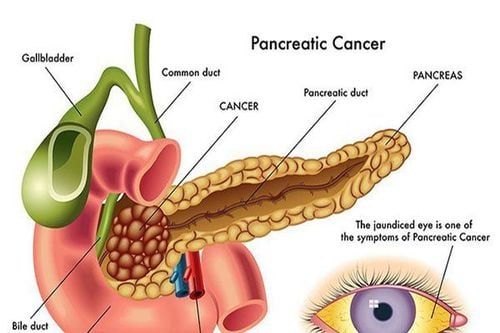
- Pancreatic cancer: Chronic inflammation in the pancreas caused by long-term pancreatitis is a risk factor for developing pancreatic cancer.
5. How is pancreatic stone treated?
Current medical perspectives generally support limiting invasive intervention for pancreatic stones when there are no complications. The occurrence of acute pancreatitis due to pancreatic stones is relatively low, while a significant number of patients have small pancreatic stones without any symptoms.
Thus, when pancreatic stones lead to pancreatitis, the patient will be hospitalized and undergo initial treatment methods such as:
- Fasting: You will need to stop eating for a few days in the hospital to give the pancreas time to recover. Once the inflammation is controlled, you may start drinking glucose water and eating porridge or thin soup. Gradually, you can return to a normal diet.
- Pain medication: Pancreatitis can cause severe pain. Your doctor will prescribe strong painkillers to help manage the pain.
- Antibiotics: Since inflamed pancreatic tissue is highly susceptible to bacterial infection from the abdominal cavity, antibiotic treatment serves both as prevention and treatment for peritonitis caused by pancreatitis.

- Intravenous fluid replacement: Since your food and fluid intake will be restricted to allow the pancreas to recover, dehydration can occur. Therefore, intravenous fluids will be administered through a vein in your arm during hospitalization. Adequate fluid supply also helps reduce the risk of acute kidney failure.
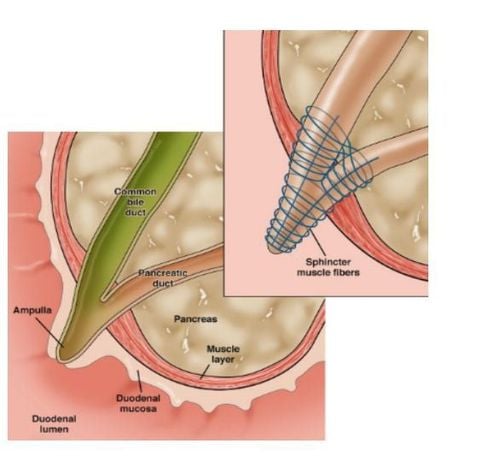
Once pancreatitis is temporarily controlled, doctors will consider treating the underlying cause of pancreatitis.Depending on the cause, different intervention methods will be chosen. Pancreatitis due to pancreatic stones is both a complication of chronic pancreatitis and a cause of recurrent acute pancreatitis. The location of the pancreatic stone determines the removal method, which could involve open surgery, laparoscopic surgery, or endoscopic retrograde techniques.
Among these, endoscopic retrograde cholangiopancreatography (ERCP) is the most commonly used method for pancreatic stone removal. This is a minimally invasive outpatient procedure that allows the patient to go home the same day. The term "retrograde endoscopy" refers to the use of an endoscope—a long, flexible, camera-equipped tube—that is inserted through the mouth, down the throat, and through the stomach to examine the pancreas, gallbladder, and bile ducts.
Small pancreatic stones can be removed using this method, while larger stones may pose challenges. However, with modern medical advancements, ERCP combined with extracorporeal shock wave lithotripsy (ESWL) is now used to break large pancreatic stones into smaller fragments, making them easier to extract.
Additionally, for chronic pancreatitis cases, patients should undergo alcohol cessation treatment. Regular alcohol consumption over many years contributes to pancreatic stone formation and chronic pancreatitis.
Moreover, patients with chronic pancreatitis often suffer from poor nutrition, in which taking synthetic pancreatic enzyme supplements is necessary to improve digestion. Taking enzyme supplements with meals can help the body better metabolize and absorb nutrients from food.
6. Lifestyle changes and prevention of pancreatic stones
After being discharged from the hospital, patients are instructed to follow recommendations to continue recovering from pancreatitis and prevent the recurrence of pancreatic stones, as well as to avoid developing them.
- Avoid alcohol consumption: If patients cannot stop drinking alcohol by themselves, doctors can suggest alcohol cessation programs.
- Avoid smoking: Patients are recommended to quit smoking. If quitting is difficult, doctors can recommend smoking cessation programs.
- Adopt a low-fat diet: Limit high-fat foods, opt for unsaturated fats, and focus on fresh fruits, vegetables, whole grains, and lean proteins in daily meals.
- Stay hydrated: Pancreatitis caused by stone formation can be due to dehydration. Staying hydrated throughout the day can support pancreatic and overall organ function.
- Exercise regularly and manage excess weight: Overweight and obese individuals are more prone to developing pancreatic and gallstones, increasing the risk of acute pancreatitis.

Pancreatic stones themselves do not cause symptoms unless they grow larger, block the pancreatic duct, and trigger pancreatitis. This condition can be extremely dangerous if not well managed. Therefore, if you have risk factors for pancreatic stone formation or have previously experienced pancreatitis, making appropriate lifestyle changes following the advice above can help prevent complications from pancreatic stones in the future.
References: ncbi.nlm.nih.gov, pancreasfoundation.org, drweil.com, cedars-sinai.org, sciencedirect.com
To arrange an appointment, please call HOTLINE or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.