Medications such as Nifedipine, Botox ®, and GTN can improve the flow through the sphincter of Oddi and reduce the symptoms of sphincter of Oddi dysfunction (SOD), but their effectiveness remains to be demonstrated in sufficiently large, randomized, and controlled trials. Therefore, endoscopic sphincterotomy remains the treatment of choice for certain patients accurately diagnosed with SOD.
1. Overview of Sphincter of Oddi Dysfunction (SOD):
The sphincter of Oddi is a muscular valve that opens and closes, allowing digestive juices, bile, and pancreatic juices to flow properly through the ducts from the liver and pancreas into the small intestine. These digestive juices are necessary for digestion.
When the sphincter of Oddi does not function properly, it fails to open when needed. There is a real blockage at the level of the sphincter, which may be due to fibrosis, inflammation, or increased sphincter tone. This prevents bile and pancreatic juices from flowing properly into the small intestine, leading to a backup of digestive juices that can cause severe abdominal pain.
Sphincter of Oddi Dysfunction (SOD) is a term used to describe various disorders of the bile ducts, pancreas, and liver caused by spasms, tightening, and dilation of this valve at inappropriate times.
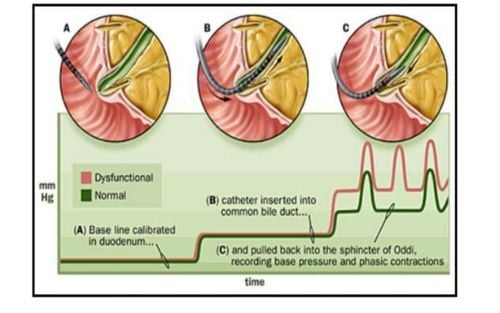
There are two types of sphincter of Oddi dysfunction (SOD). One occurs when digestive juices reflux into the bile ducts in the liver, causing 'biliary dysfunction'. The other occurs in the pancreas, causing inflammation known as 'pancreatitis'. These two types of sphincter of Oddi dysfunction can be divided into three categories. In type I, patients experience pain, abnormal blood test results, slow drainage of contrast dye during ERCP, and abnormal imaging findings (dilation of the common bile duct and dilation of the pancreatic duct for type 1). In type II, patients experience pain and only one or two of the previous criteria. With type III dysfunction, there are no clear laboratory findings or abnormalities, and the only sign of the problem is abdominal pain.
Diagnosing type III sphincter of Oddi dysfunction is more challenging than other types and may be more difficult to treat, as the percentage of patients improving after therapies is lower.
2. Treatment of sphincter of Oddi dysfunction (SOD) with medication
Some exogenous agents relax the sphincter of Oddi, reducing its pressure and resistance. These include calcium channel blockers, tricyclic antidepressants, Botox, glyceryl trinitrate (GTN), and somatostatin.
Nifedipine has been shown to counteract the effects of opiates on the sphincter of Oddi and improve pain associated with sphincter of Oddi dysfunction (SOD) in a short-term study. Injecting Botox® into the sphincter of Oddi through a sclerotherapy needle reduces sphincter pressure by 50% for four months, followed by a 50% improvement in bile flow in two patients with post-cholecystectomy pain and increased sphincter of Oddi pressure. GTN has been used to assist in the removal of common bile duct stones formed without the need for endoscopic papillary dilation or endoscopic sphincterotomy and reduces both the baseline sphincter of Oddi pressure as well as the amplitude and frequency of sphincter of Oddi contractions in a non-randomized controlled clinical trial. Intravenous somatostatin has been shown to reduce the average baseline sphincter of Oddi pressure in patients with acute alcohol-induced pancreatitis.
A prospective study on patients with biliary sphincter of Oddi dysfunction (SOD) (identified by clinical and laboratory data) evaluated the combination of low-dose tricyclic antidepressants, nifedipine, and GTN. If there was no improvement after 3-6 months, patients were offered biliary sphincterotomy. 51% of patients (76% with type III) improved or had symptom improvement with medical treatment alone, 12% improved or resolved symptoms with sphincterotomy, and 10% improved with both medical therapy and sphincterotomy. Despite the promise, opiates were still allowed in this study, confounding the identification of symptom improvement due solely to the interventions.
3. Treatment of sphincter of Oddi dysfunction (SOD) with procedures
Non-drug treatments for sphincter of Oddi dysfunction (SOD) are commonly used, particularly endoscopic sphincterotomy for patients with biliary type I and II SOD and pancreatic SOD. Pain relief has been demonstrated in 90% of biliary type I and 70% of type II patients. However, it is ineffective and may be harmful in type III patients. The evaluation of predictive factors and interventions in the sphincter of Oddi dysfunction trial is a landmark study for treating type III. This is a multicenter, randomized, sham-controlled trial in patients with post-cholecystectomy pain, no imaging or laboratory abnormalities, and no prior Oddi sphincter treatment. Participants underwent either sphincterotomy or sham sphincterotomy for abdominal pain. Investigators concluded that performing sphincterotomy in type III SOD patients is ineffective. Therefore, endoscopists are increasingly moving away from performing sphincterotomy in these patients.
4. Conclusion
Sphincter of Oddi dysfunction (SOD) represents impaired fluid flow through the sphincter of Oddi due to fixed narrowing or impaired muscle control (dyskinesia). Gallbladder function appears to play an important role in the sphincter of Oddi mechanism, and patients without a gallbladder are more likely to develop SOD. Other potential contributing factors include female gender, hypothyroidism, irritable bowel syndrome, previous pancreatitis, and exogenous drugs. Data demonstrating the relationship between opioids and SOD are clear and reproducible. Clinical syndromes resulting from this, especially in post-cholecystectomy patients, include abdominal pain accompanied by sudden but reversible elevation of liver enzymes and acute pancreatitis. Different opioid agents seem to have varying effects on the baseline and phase contractions of the sphincter of Oddi. While exogenous mu-opioid agonists negatively affect the flow through the sphincter of Oddi, there is some evidence that nifedipine, Botox®, and GTN may improve flow through the sphincter of Oddi and alleviate symptoms of SOD. However, the effectiveness of these agents remains to be demonstrated in sufficiently large, randomized, and controlled trials. Endoscopic sphincterotomy remains the treatment of choice for certain patients accurately diagnosed with SOD. Nevertheless, raising awareness among caregivers about the risk factors for SOD creates opportunities for diagnosis and intervention, including avoiding potential precipitating agents, especially in the absence of a gallbladder.
References:Elham Afghani. Sphincter of Oddi Function and Risk Factors for Dysfunction. Front Nutr. 2017; 4: 1. Williamson JB. Effect of morphine after cholecystectomy. Br Med J (1941) 1:215.10.1136/bmj.1.4179.215-a [CrossRef] [Google Scholar] Smyth MJ. Exploration of the common bile duct for stone. Drainage with T-tube and cholangiography. Br Med J (1941) 1:111–26.10.1136/bmj.1.4177.111 [PMC free article] [PubMed] [CrossRef] [Google Scholar] Eichhorn EP, Jr., Boyden EA. The choledochoduodenal junction in the dog; a restudy of Oddi's sphincter. Am J Anat (1955) 97:431–59.10.1002/aja.1000970305 [PubMed] [CrossRef] [Google Scholar]
To arrange an appointment, please call HOTLINE or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.