Alternatives of epidural analgesia
Posted by Doctor Nguyen Thi Hoai Nam - Department of Surgical Anesthesia, Vinmec Central Park International General Hospital.
It is worth emphasizing that the advantages of epidural analgesia on cardiovascular, respiratory, gastrointestinal are noted in major surgery, open surgery. The majority of recommendations no longer recommend epidural analgesia for laparoscopic surgery such as cholecystectomy and colectomy. Furthermore, these advantages are only apparent when compared with systemic opioid use.
1. Alternatives to Epidural Anesthesia
There is increasing evidence from meta-analyses and systematic reviews that safer and more effective alternatives to epidurals are being used in major thoracic, abdominal, and orthopedic surgery.
These alternative methods of analgesia include:
Paravertebral anesthesia for thoracic surgery Peripheral nerve anesthesia for hip and knee replacement Intravenous lidocaine for colorectal surgery Intraoperative catheter infusion for many surgeries including abdomen , Cardiology, Vascular Surgery Major abdominal surgery, transverse abdominal plane block (TAP block) for abdominal wall related surgery...
2. Peripheral nerve anesthesia techniques
In recent years, peripheral nerve blockade continues to thrive as an efficacious and safe technique, providing better pain relief than opioids. Regardless of catheter placement, continuous peripheral nerve blockade provides better analgesia and reduced opioid use and results in a lower incidence of opioid side effects such as postoperative nausea and vomiting, and sedation.
There is strong evidence that some peripheral nerve anesthesia techniques are as effective as epidurals, but with a better side effect. This is supported by the evidence-based recommendations of the Anesthesiologists at the Universities of Australia and New Zealand. Furthermore, the PROSPECT team did not recommend epidural analgesia as the first choice for patients with hip or knee replacement. Two meta-analyses concluded that peripheral nerve blockade is superior to epidural anesthesia after major knee surgery.
Interestingly, another meta-analysis of 16 RCTs concluded that 1-dose femoral nerve block is superior to epidural analgesia and that there is no further benefit in adding sciatica block or having an injection technique. continuous transmission. In summary, there is growing evidence that the peripheral nerve block technique is superior to epidural analgesia for patients with total hip or knee replacement.
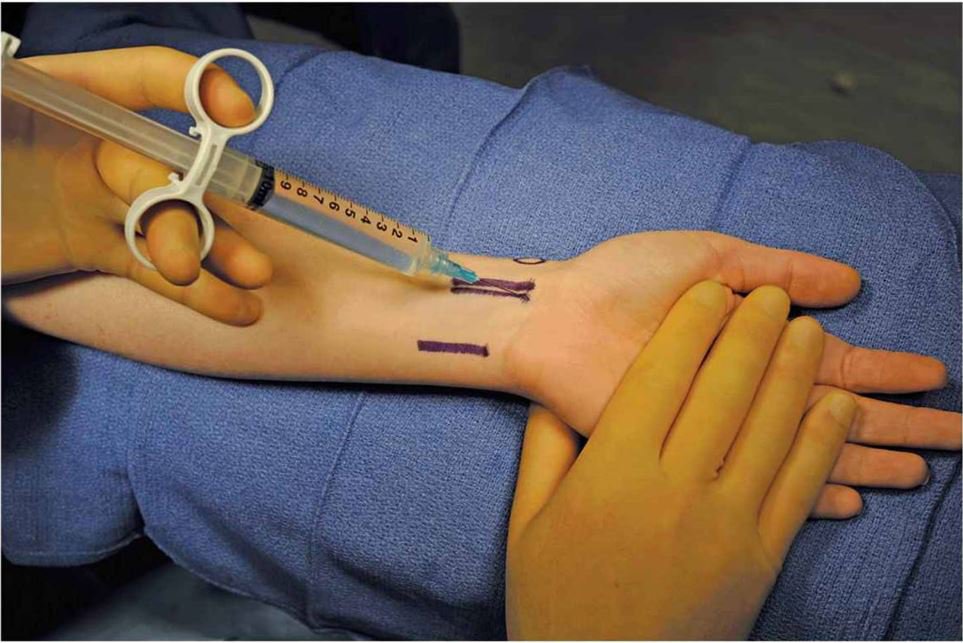
Kỹ thuật gây tê thần kinh ngoại biên vị trí cổ tay
3. Live edge numbness
A systematic review found that both epidural and paraspinal analgesia provide equivalent analgesia up to 48 h after thoracotomy, but paraspinal anesthesia reduces the incidence of respiratory complications, urinary retention, hypotension, and vomiting. and postoperative nausea. The PROSPECT team evaluated local anesthetic techniques for post-thoracotomy pain based on data from 74 RCTs and concluded that paravertebral anesthesia was as effective as thoracic epidural analgesia but with a lower incidence of hypotension.
4. Infusion through the incision catheter
This technique is well practiced in postoperative pain management in both inpatients and emergency rooms. A systematic review of 39 RCTs, including 15 cardiothoracic surgery RCTs and 16 major orthopedic surgery RCTs, showed that postoperative pain management by intraoperative catheter infusion reduced pain scores at rest and during activity, and decreased need for postoperative pain. opioid requirements, reduce postoperative nausea and vomiting, and increase patient satisfaction. The authors concluded that “the most striking feature is the consistent evidence of these benefits across a wide range of surgeries, incision catheter placement and dosing regimens associated with a low rate of complications related to surgery. catheters. Both the effectiveness and simplicity of this technique encourage its widespread clinical use.”
Similar conclusions can be drawn from evidence-based data from a group of anesthesiologists from the Universities of Australia and New Zealand. A more recent meta-analysis and related article were less positive, but these conclusions are most likely due to the exclusion of orthopedic and true non-incisional catheter patients. In clinical practice, incisional catheterization techniques include catheters that are placed through the incision into deeper layers or compartments such as the subfascia, peritoneum, intraosseous, and intraarticular. The importance of appropriate catheter placement was demonstrated in a study of patients undergoing colorectal surgery.
Intraperitoneal catheter ablation is effective in analgesia up to 72 hours, reduced opioid consumption, earlier recovery of bowel function and shorter hospital stay of 30 hours. Similarly, incisional anesthesia with catheter placed under the fascia in pain relief after cesarean section is as effective as an epidural. This conclusion is supported by 1 Cochrane study. Evidence-based PROSOECT recommendations include incisional anesthesia for inguinal hernia surgery, cholecystectomy, laparoscopic hysterectomy and colectomy (peritoneal anesthesia), total knee replacement, and total hip replacement. section, and cut hemorrhoids. This technique is also recommended by the ASA Practice Guidelines as part of a multimodal analgesia regimen for postoperative pain management.

Truyền qua catheter vết mổ được ứng dụng trong phẫu thuật thoát vị bẹn
Incisional catheter analgesia is recommended in the Australian and New Zealand University Anesthesiology Practice Guidelines 2nd (2005) and 3rd Edition (2010) based on Level 1 evidence. However, many questions remain to be answered. Responses include optimal catheter placement in different surgeries, local anesthetic concentrations and volumes, risk of local anesthetic toxicity, and the potential role of supportive therapies. or without a catheter is simple, safe, and effective for many but not all surgeries. They can be used alone or as part of a balanced, multimodal analgesia regimen. A detailed comparison of alternative analgesia techniques is needed to identify which is the most clinically effective, cost-effective for different surgeries.
5. TAP Block
This is a relatively new technique showing promising efficacy in pain management in patients with major laparotomy and gynecological surgery. A few other additions to the technique, with or without guided ultrasound have been reported. A recent review of RCTs showed a clinically significant reduction in opioid requirements and pain, both at rest and during exercise, as well as a reduction in opioid side effects such as sedation, nausea, and vomiting. This advantage is demonstrated in colectomy, cesarean section, abdominal hysterectomy, open appendectomy, and laparoscopic cholecystectomy. The authors conclude, “Treatment of postoperative pain with TAP block is a promising new technique, which has demonstrated a reduction in opioid consumption as well as an improved pain score in operations involving the anterior abdominal wall. More studies are needed to confirm these findings.
6. Local anesthetic to relieve pain
Kerr and Kohan developed local permeation analgesia (LIA) as part of an analgesia regimen after hip and knee replacement. It is a 5-step technique based on infiltration of a mixture of Ropivacaine 0.2%, ketorolac and epinephrine. Using the “moving needle” technique, a large amount (up to 150ml) of 0.2% ropivacaine is injected into the tissue area just below the incision. An intra-articular catheter gives a single dose 15-20 hours postoperatively. Surgery was performed under spinal anesthesia.
In a study of 325 hip or knee replacement surgery patients, the majority had low pain scores and were able to be discharged overnight. Mean duration of independent movement was less than 25 hours in a cohort study and less than 20 hours for total knee replacement. LIA has received a lot of attention, especially in Scandinavian countries, Great Britain, and Australia. In Sweden, 75% of total knee replacements were performed with LIA in 2009.
In a study of 325 hip or knee replacement surgery patients, the majority had low pain scores and were able to be discharged overnight. Mean duration of independent movement was less than 25 hours in a cohort study and less than 20 hours for total knee replacement. LIA has received a lot of attention, especially in Scandinavian countries, Great Britain, and Australia. In Sweden, 75% of total knee replacements were performed with LIA in 2009.

Kỹ thuật giảm đau tê thấm tại chỗ (LIA) được ứng dụng trong phẫu thuật thay khớp gối toàn bộ
Several published studies have shown impressive results and shorter hospital stays, although this is longer than initially reported by Kerr and Kohan. Local anesthetic pain relief is better than epidural after total hip replacement and better than femoral nerve block and spinal morphine after total knee replacement. Another study found that LIA was better than epidural analgesia in the first 24 hours after surgery, better knee function, earlier mobility, and 2 days earlier hospital discharge. A recent review of LIA concluded that LIA has a role in total knee replacement but not total hip replacement and that gabapentin is probably the better alternative. A related article disagrees and concludes that LIA is probably still the better choice due to its reduced side effects. However, many questions need to be noted and answered, including: the role of local anesthetic of ketorolac and epinephrine, the role of compression and ice, and the role of surgical technique. Furthermore, it is important to define what exactly the “LIA technique” is because there are many variations that make comparisons difficult across studies.
7. Is epidural analgesia still indicated?
Raw data clearly demonstrate excellent epidural analgesia. In patients with open major vascular surgery and in high-risk patients undergoing other major surgery, epidural analgesia with local anesthetic reduces the incidence of cardiovascular and respiratory complications. Currently available evidence suggests that regional anesthesia is superior to opioid analgesia. In well-equipped centers, epidural analgesia remains a good choice during the transition when evidence-based alternatives such as peripheral neuropathy, paravertebral anesthesia, LIA, and catheters are used. incision and TAP block are being introduced into clinical practice.
8. Conclusion
Recently reported evidence suggests that epidural analgesia is not as significant as previously assessed. Although the analgesic effect may be prominent and has the advantage of reducing cardiovascular and respiratory complications in patients at high risk of major vascular surgery or open heart surgery, epidurals are generally decreasing. Some reasons for this decrease in the use of this invasive, cost-effective and experiential technique:
There is little evidence of a reduction in postoperative mortality associated with epidural analgesia. There is little convincing evidence of a reduction in complications in the low-to-moderate-risk surgical group. Advances in surgical technique such as many surgeries previously performed only on inpatients are now performed in patients who operate on the same day or only 1 night in the hospital.

Người bệnh được mổ trong ngày và chỉ cần một đêm nằm viện theo dõi sau mổ
Use fast postoperative recovery protocols, no epidural, early mobilization. Widespread implementation of prophylactic anticoagulation regimens Increasing evidence that alternative, less invasive regional anesthetic techniques provide even greater pain relief than epidurals after most major surgeries Lack of conclusive evidence on cost-effectiveness of epidural analgesia despite decades of practice. Worry about litigation related to serious neurological complications. It is therefore not an exaggeration to suggest that the diminishing role of epidural analgesia can be expected to further diminish. Epidural analgesia remains the gold standard in pain relief during childbirth because there is currently no good alternative. Epidural analgesia is no longer the gold standard in postoperative analgesia. Continued use of epidural analgesia in your institution should be based on a careful assessment of the risks and benefits of the method from reported local data, rather than traditionally being considered old fashioned.
Translated by Narinder Rawal, MD, PhD, Epidural Technique for Postoperative Pain Gold Standard No More?, (Reg Anesth Pain Med 2012;37: 310 - 317)






