Anesthesia resuscitation in ischemic cardiomyopathy and coronary reperfusion - Part 2
Posted by Doctor Ho Thi Xuan Nga - Cardiovascular Center - Vinmec Central Park International General Hospital
More than 60% of vascular surgery patients have signs of coronary artery disease and the rate of postoperative infarction is between 4.7 and 8.5%. However, this type has a very high risk of ischemia, accounting for up to 10% of all surgical patients.
1. Postoperative Infarction in Cardiac Surgery Preoperative clinical status is a major risk factor for postoperative complications in coronary revascularization (PAC: coronary artery bypass grafting) . Different risk indices are used to predict severity as follows:
Cardiogenic shock or ventricular dysfunction (EF <0.35); Preoperative acute ischemia or infarction, unstable angina; Common trunk injury or proximal IVA; Emergency surgery or reoperation; Comorbidities: kidney failure, diabetes; Polyvascular artery disease; Age > 70 years old; Female gender. 2. Ischemia and reperfusion 2.1 Hibernation: A form of self-protection in which the ischemic myocardium becomes inotropic in order to adjust its mVO2 requirement with a low DO2 supply. Range is variable, but no necrosis; the function of this myocardium can be stimulated by catecholamines; it is reversible in case of revascularization (from a few hours to several days).

Hình thức ngủ đông trong thiếu máu cục bộ
2.2 Injury reperfusion When a large supply of O2 releases superoxide and cytotoxic free radicals and is accompanied by hypercalcemia. Although the pressure is normal, the blood flow is excessive compared to the maximal vasodilation of the ischemic areas. Causes common, but reversible, malignant ventricular arrhythmias.
2.3 Myocardial stupor Is the persistence of myocardial dysfunction after revascularization while perfusion is restored; the duration is from a few hours to a few days; function can be stimulated by catecholamines.
2.4 No reperfusion No distal outflow into the myocardium while epicardial outflow is restored.
3. Intraoperative and postoperative management of ischemia and infarction During the operative period, the presence of electrical changes to the ECG (ST segment elevation or depression, bundle branch block) left) and/or elevation of cardiac enzymes should be clinically managed similarly to those recommended for STEMI or non-STEMI infarction:
General measures:
Deep anesthesia or analgesia; Maintain PAM > 80 mmHg; Ventilate with FiO2 0.8 - 1.0; Optimized Hb (> 100 g/L); Take a blood sample to determine the cardiac enzyme troponin and CK-MB; Antiplatelet: Aspirin 500 mg IV Ticagrelor (180 mg po/nasogastric tube); if contraindicated or not available: clopidogrel (300-600 mg po/nasogastric tube). Anticoagulation: Unfractionated heparin (bolus 60 IU/kg, continuous infusion at 12-15 IU/kg/hour) or bivalirudin (2 mg/kg/hour), or fondaparinux (scut 2.5 mg) or enoxaparin ( 1 mg/kg/12 hours).

Sử dụng thuốc Aspirin 500 mg IV trong xử trí thiếu máu cục bộ và nhồi máu
Other treatment:
Noradrenaline (0.03-0.5 mcg/kg/min); Nitroglycerin (5-20 mcg/kg/min); Atorvastatin (20 mg orally/nasogastric tube), simvastatin (20 mg). Hemodynamically stable patients or in cases of tachycardia/arrhythmia
β-blockers: metoprolol, atenolol, bisoprolol or other selective β-blocker: oral or intravenous; During anesthesia: bolus and / or infusion of esmolol; Contraindications: atrioventricular block, cardiogenic shock. Hemodynamically unstable patients
Catecholamines stimulate α and β; Intra-aortic balloon counterpulsation; Coronary angiography (dilation and stenting); Within 90 minutes if STEMI; Within 12-24 hours if non-STEMI angina or unstable angina. 4. Complications of acute coronary syndromes: SCA Several serious complications threaten patients in the days following SCA, especially STEMI types.
Cardiogenic shock and ventricular failure : Aortic balloon counterpulsation is the method of choice to reduce ventricular output (T) and improve coronary perfusion without increasing mVO2; Cardiac arrhythmias: atrial fibrillation, atrioventricular conduction block, tachycardia or ventricular fibrillation; Mitral regurgitation due to ventricular dilatation (T): transmural ischemia or rupture of papillary muscle; in severe mitral regurgitation, contrast balloon placement is effective in pending surgical repair; Ventricular septal defect: need to close the ventricular septal defect by surgery; Ventricular rupture (T): most often fatal by acute cardiac tamponade; Ventricular aneurysm (T): ACE inhibitors inhibit ventricular remodeling (T), but surgical excision of the aneurysm is usually necessary; Thrombosis in the left ventricular chamber : it usually occurs in the hypodynamic area, most often at the apex; Anticoagulation is required for at least 6 months.
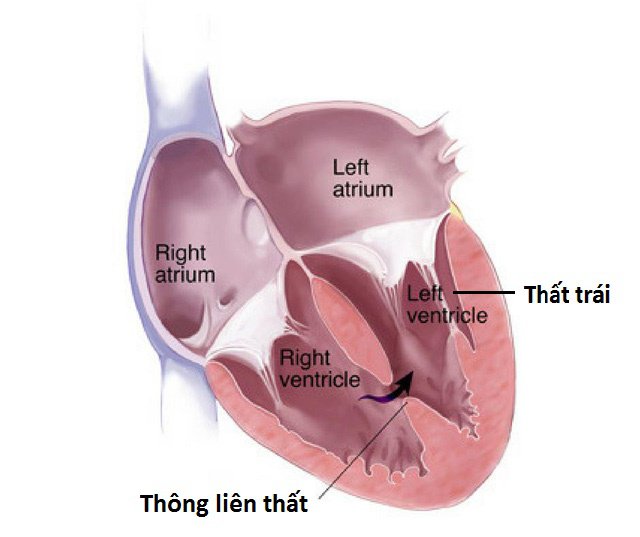
Lỗ thông liên thất cần được đóng lại bằng phương pháp phẫu thuật
5. Preoperative evaluation of coronary patients Cardiovascular examination and stress testing in the absence of treatment change are not necessary. They are indicated only in patients with stage III-IV angina, ventricular dysfunction, or severe arrhythmia.
Pending surgery, the heart rate of coronary patients should be closely controlled at 60-65 beats/min (β-blocker).
Preoperative prophylactic reperfusion does not make sense; the indications for revascularization (PCI + stent or PAC) are the same outside the surgical setting:
Unstable coronary artery disease (stage III-IV angina); Persistent angina despite maximal treatment; High-risk injury. In stable (stages I-II) coronary artery disease, even more severe, optimal medical therapy (β-blockers, antiplatelet agents, statins) is preferable to revascularization.
Any coronary revascularization must have a limited surgical delay time limit; After this time, cardiovascular risk increases 5-10 times.
When patients require surgical treatment for a short time (<4 weeks), optimal medical therapy (β-blocker, antiplatelet agent, statin) is preferable to attempting revascularization, even when coronary artery disease is unstable.
Current priorities for optimal continuous medical cardioprotective therapy are preoperative exploration and revascularization.
6. Preoperative coronary revascularization Death from revascularization and surgery is approximately the same. Cardiac risk was greatly increased 6 weeks after revascularization (25% mortality rate). Benefits appeared only after 3 months (mortality <1%). For active stents (DES), benefits appeared only after 12 months. Stable angina (I-II) is not an indication for revascularization.

Người bệnh có thể xuất hiện tình trạng đau thắt ngực ổn định
7. Time limit for performing noncardiac surgery after revascularization: Simple angioplasty 2-4 weeks.
Simple metal stents (BMS, passive stents) or coronary artery bypass graft surgery.
Major surgery: 6 weeks; Elective surgery: 3 months. Drug-eluting stents (DES; active stents)
Major surgery: 12 months; Elective surgery: 6 months. Recommended duration of antiplatelet therapy after a coronary event:
Clopidogrel (75 mg/day), prasugrel (10 mg/day) or ticagrelor (2 x 90 mg/day): Simple balloon dilation:2 week; drug-coated balls: 3 months; Passive elective stents 4-6 weeks; in case of acute coronary syndrome: 12 months; Infarction 3-6 months; Stents work 6-12 months (>12 months if very high risk); Acute coronary syndrome: 12-month conservative treatment with aspirin (75-325 mg/day) without interruption. Recommendations for preoperative interruptions for antiplatelet agents:
Aspirin : No interruption in principle; if necessary: stop 5 days Clopidogrel : Stop 5 days Prasugrel: Stop 7 days Ticagrelor: Stop 5 days; If urgent, stop for 3 days

Một số loại thuốc được khuyến cáo cần dừng trước giai đoạn phẫu thuật
Please see more articles about "Resuscitation anesthesia in ischemic cardiomyopathy and coronary reperfusion" by Doctor Ho Thi Xuan Nga:
Anesthesia resuscitation in ischemic and reperfusion cardiomyopathy Coronary Anesthesia - Part 1 Anesthesia resuscitation in ischemic cardiomyopathy and coronary reperfusion - Part 2 Anesthesia resuscitation in ischemic cardiomyopathy and coronary reperfusion - Part 3 REFERENCES
FLEISHER LA , BECKMAN JA, BROWN KA, et al. ACC/AHA 2007 Guidelines on perioperative cardiovascular evaluation and care for non-cardiac surgery: Executive summary. J Am Coll Cardiol 2007; 50:1707-32 GROSSMAN W, ed. Cardiac catheterization and angiography. 3rd edition. Philadelphia, Lea and Febiger, 1986, 378 KAPLAN Joel.A, Cardiac Anesthesia for cardiac and non-cardiac surgery, 7th edition. Elservier, 2017, 1453-236 KERTAI MD, BOUTIOUKOS M, BOERSMA M, et. Aortic stenosis: An underestimated risk factor for perioperative complications in patients undergoing noncardiac surgery. Am J Med 2004; 116:8-13 KWAK J, ANDRAWES M, GARVIN S, et al. 3D transesophageal echocardiography: a review of recent literature 2007-2009. Curr Opin Anesthesiol 2010; 23:80-8 MILLER FA. Aortic stenosis: Most cases no longer require invasive hemodynamic study. J Am Coll Cardiol 1989; 13:551-8 STS – Society of Thoracic Surgeons National Cardiac Surgery Database, 2005. http://www.sts.org/documents/pdf/STS-ExecutiveSummary.pdf TIMMIS SB, KIRSH MM, MONTGOMERY DG, STARLING MR. Evaluation of left ventricular ejection fraction as a measure of pump performance in patients with chronic mitral regurgitation. Cathet Cardiovasc Intervent 2000; 49:290-7 TORNOS MP, OLONA M, PERMAYER-MIRALDA G, et al. Heart failure after aortic valve replacement for aortic regurgitation: prospective 20-year study. Am Heart J 1998; 136:681-7






