Brugada syndrome is one of the leading causes of sudden death
The article was written by Specialist Doctor II Nguyen Bang Phong - Cardiovascular Center - Vinmec Times City International General Hospital.
Sudden death often occurs in people with structural heart disease, especially coronary artery disease. However, about 5-10% of sudden deaths occur in people without structural cardiac abnormalities and coronary artery disease, but may have risk factors for arrhythmias such as long QT syndrome. , short QT syndrome, pre-excitation syndrome, concussion (commotio cordis) and Brugada syndrome.
1. Epidemiology
Brugada syndrome was first mentioned in 1991, consisting of characteristic electrocardiographic changes and severe ventricular arrhythmias causing syncope or sudden death. The Brugada-shaped transformation on the electrocardiogram is quite similar to the right bundle branch block in leads V1, V2 due to a characteristically elevated J-score. (Figure 1).
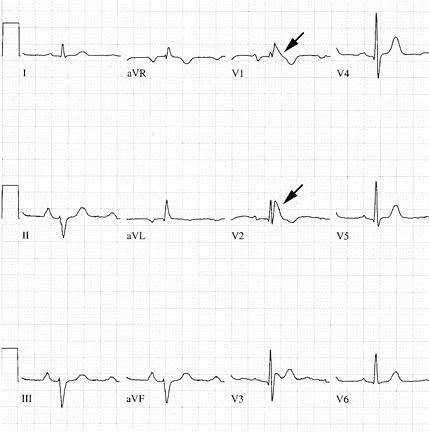
Many cases have only Brugada-form changes on electrocardiogram without symptoms (persistent ventricular tachycardia, life-saving cardiac arrest or sudden death), then not called Brugada syndrome but electrocardiogram Brugada pattern.
According to some statistics, in the US, about 0.1 - 0.4 % of the population have Brugada-type ECG changes. South Asia, especially Southeast Asia, has the highest rate of sudden death from Brugada syndrome in the world. Statistics also show that the proportion of men with Brugada syndrome is 2 to 9 times higher than that of women. The reason for this difference is not clear. Experimental studies have shown a relationship between the male sex hormone testosterone and the activity of ion channels in the heart. Clinical observations also show that the frequency of electrocardiograms with Brugada-form changes in schizophrenia is higher than in normal people: 11.6% versus 1.1%.
2. Pathogenesis
The pathogenesis of Brugada changes on electrocardiogram and ventricular arrhythmias has not been fully elucidated. The researchers found in patients with Brugada syndrome mutations in the genes SCN 5A and SCN 10A that act on sodium channels in the heart. Sodium channels are concentrated mainly in the right ventricular epicardium.
Abnormal activity of these channels increases the dispersion of repolarization, resulting in transmural potential gradients, resulting in characteristic ST elevation in the right precordial leads and, if present An extrasystole at the time of vulnerable repolarization can cause ventricular fibrillation. Abnormalities of sodium channels also increase the heterogeneity of the refractory period of the myocardium.
Predisposing factors for the onset of clinical symptoms (persistent ventricular tachycardia, sudden cardiac arrest) are fever, atrial fibrillation, some psychotropic drugs, some anesthetics, cocaine, antipsychotic drugs. Heart rhythm has inhibitory effects on sodium channels such as Ajmaline, Flecainide, Procainamide, Propafenone...

Sốt là một trong các yếu tố tạo thuận lợi để khởi phát các triệu chứng lâm sàng
3. Clinical situation
There are 3 situations:
Only Brugada transformation in diabetes, persistent ventricular tachycardia, no syncope. Discovered by chance, either through screening when someone in the family has Brugada syndrome.., or going to a cardiologist because of palpitations. Diabetes with Brugada form, life-saving syncope or ventricular fibrillation. Electrocardiogram with Brugada form, sudden death.
4. Treatment
The goal of treatment for patients with Brugada syndrome is to prevent sudden death.
To date, antiarrhythmic drugs (except for two drugs Quinidine and Amiodarone) have proved ineffective, even causing the onset of serious ventricular arrhythmias, especially sodium channel blockers as described above. said above. Quinidine has been shown to be more effective than amiodarone in preventing dangerous ventricular arrhythmias in patients with Brugada syndrome, in addition to having fewer side effects than amiodarone with prolonged use.
Abortion of the arrhythmogenic area according to the electrical map made in the right ventricular outflow tract and the right ventricular free wall is a technique that is being evaluated because the number of patients applying this technique is still small. .
The most effective measure to prevent sudden death for patients with Brugada syndrome is the implantation of an automatic defibrillator (ICD). The ICD can detect ventricular arrhythmias and will act automatically according to the arrhythmic signal it receives: asynchronous shock if it is a ventricular fibrillation, or an overfrequency lead if it is a ventricular tachycardia. When the pacemaker exceeds the frequency by about 3-5 times without stopping the ventricular tachycardia, the ICD will switch to synchronized shock mode.

Máy khử rung tự động (Impantable Cardioversion Defibrillator: ICD)
This is a fairly expensive, but most effective, technique, indicated for patients with Brugada syndrome who have had syncope due to ventricular tachycardia, or who have had a life-saving cardiac arrest. Patients with Brugada-type electrocardiogram, with palpitations, when electrophysiological examination shows ventricular tachycardia, should also consider implanting an ICD. Current ICD machines have a battery life of about 7 years.
According to statistics at Vinmec Times City hospital, from September 11, 2017 to April 19, 2018, the hospital has implanted 25 ICDs, including 11 patients with Brugada syndrome, accounting for 44%, the average age average is 42.1. After implantation of the ICD, the patients were stable. Routine machine testing in the first year showed that: there were 3.5 times of ventricular fibrillation with successful defibrillation in 6 patients, in particular, there were patients with 12 episodes of ventricular fibrillation in 24 hours who were successfully defibrillated, or in other words this patient has been saved 12 times. Among the remaining 6 patients, 4 patients with an average of 2.5 episodes of ventricular tachycardia were successfully conducted over-rate. Only 2 patients did not see ventricular arrhythmias during the first year of follow-up.
Để đặt lịch khám tại viện, Quý khách vui lòng bấm số HOTLINE hoặc đặt lịch trực tiếp TẠI ĐÂY. Tải và đặt lịch khám tự động trên ứng dụng MyVinmec để quản lý, theo dõi lịch và đặt hẹn mọi lúc mọi nơi ngay trên ứng dụng.






