Value of thyroid FNA test?
Article written by MSc Bui Thi Hong Khang - Pathologist, Laboratory Department - Vinmec Central Park International General Hospital
Fine-needle aspiration cytology or FNA for short applied in pathological diagnosis of thyroid nodules is considered the most effective method due to its accuracy of over 95%; with positive predictive value from 89-98%, negative predictive value 94-99%; false negative and false positive rate less than 1%. FNA has helped to select the right cases for surgery, reducing the number of surgical cases by more than half, which means saving treatment costs.
1. How is the thyroid FNA technique performed?
Simple thyroid FNA technique that can be easily performed in a routine clinic for palpable thyroid nodules. For lumps that are too small to be palpated, an ultrasound-guided FNA should be performed. (Figure 1).

Hinh 1: Kỹ thuật thực hiện FNA 1 cục trong tuyến giáp (A); Tế bào lấy ra được trải lên tiêu bản (B); đối với các cục nhỏ, FNA được làm dưới siêu âm giúp đưa kim hút vào đúng vị trí tổn thương (C).
Removed cells were spread onto the slide, fixed immediately with 95% alcohol and stained by Papanicolaou method (or allowed to air dry if stained by May-Grnwald-Giemsa, Diff-Quik method). The cell morphological changes observed under light microscopy allow the diagnosis of thyroid lesions as benign, malignant or suspected malignancy.
2. How are thyroid FNA test results done?
The terms used to describe the diagnostic results of thyroid FNAC may vary from laboratory to laboratory, country to country; This confuses clinicians in choosing treatment.
Therefore, in 2007, the US National Cancer Institute proposed the Bethesda system of thyroid cytology, in order to unify the terminology, description and classification of lesions into 6 diagnostic groups.
3. Significance of the Bethesda system of thyroid cytology
This system helps clinicians easily choose the appropriate treatment, as well as facilitates the exchange of experience among cytologists.

chẩn đoán Nguy cơ ác tính (%) Hướng xử trí
4. How normal is thyroid cytology?
According to the Papanicolaou staining method, normal thyroid cysts are spherical bodies with an average diameter of 200 μm (50-500 μm), which rupture when aspirated, forming flat 2-dimensional honeycomb-like clusters, including Thyroid follicular cells of uniform size are linked together.
Thyroid follicular cells have round nuclei, 7-8 μm in diameter, regular nuclear membrane, coarse granular chromatin, relatively hyperchromatic, nucleoli indistinct; cytoplasm is pale green; Cell limits are not obvious. Because the cytoplasm of thyroid follicular cells is fragile, the bare nuclei can be seen as round, easily mistaken for lymphocytes. Thyroid colloid is found in the matrix between follicular cells, whose characteristics vary according to the functional status of the thyroid gland.
The less active the thyroid gland, the thicker the colloid, pink or blue, with irregular undulations; Thyroid gland is overactive, the colloid has a thin water-like consistency, which is pink or very pale blue, difficult to see. (Figure 2).
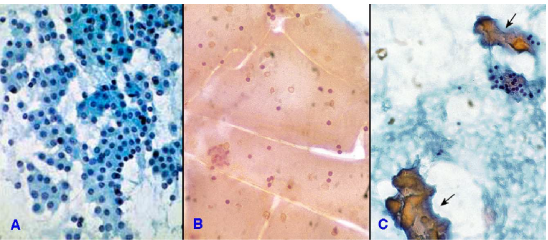
Hình 2: Tế bào nang giáp xếp thành đám phẳng hình tổ ong (A); chất keo loãng (B); chất keo đặc (mũi tên) (C).
5. Learn the results groups of the Bethesda system for diagnostic thyroid cytology
5.1 Group I - Nondiagnostic/Unsatisfactory This group was created to exclude specimens that did not meet the requirements of quality (smear too thick, bloodstained; poor fixation) and number (small cell count), which, if still used diagnostically, increases the incidence of false negatives. (Figure 3)

Hình 3: Phết không đủ tiêu chuẩn chẩn đoán: quá dầy, nhiều máu (A)
To meet diagnostic criteria, each slide must contain ≥ 6 groups of follicular cells, with each group having ≥ 10 cells. However, this quantitative criterion will be waived for the following 3 cases:
The specimen contains atypical follicular cells, even if the number is small, it is still considered to meet the diagnostic criteria. For example, a slide containing only a group of follicular cells forming a papillary structure with the morphological features of papillary thyroid carcinoma is sufficient to be classified as group VI. Specimens containing high levels of lymphocytes (from Hashimoto's thyroiditis), polymorphonuclear leukocytes (acute abscessed thyroiditis), epithelial cells, and macrophages (granulomatous thyroiditis) were still considered diagnostic criteria. diagnosis (group II) even though only few follicular cells were present. A specimen containing all the solid thyroid colloid (from a multinodular thyroid aneurysm) was also considered to meet the diagnostic criteria (group II) even though it contained few follicular cells. The number of aspiration cases falling into group I accounts for about 10-30%, depending on each cytological labor; but once the rate is more than 20%, it is necessary to check the quality of technical stitches (aspiration, fixation and dyeing...) to achieve optimal results. Management attitude for group I is to repeat FNAC for the second time after 3 months under ultrasound guidance; about 60% of second FNAC meet diagnostic criteria.
5.2 Group II - Benign Thyroid pathologies with benign cytological findings are most commonly polygranulomatous thyroiditis, Hashimoto's thyroiditis, granulomatous thyroiditis and acute thyroiditis.
5.3 Group III - Atypia of Undetermined Significance Classified in this group are specimens containing a number of abnormal cells that are not known to be benign or malignant (including follicular cells). thyroid and other cell types) but do not meet the criteria for group IV, V or VI; The patient will be asked to repeat the FNAC after 3 months. The risk of malignancy in group III is 5-15%.
It is necessary to avoid overusing diagnosis of group III because in many cases, atypical cells are caused by technical errors in specimen preparation (slow fixation, drying,...). The prevalence of group III should not exceed 7% of all FNAC cases.
The characteristics of the specimens that can be classified into group III are very diverse, including: (Figure 9)
Beside the 2-dimensional flat clusters, there are small thyroid cysts with equal proportions (50/50); Small thyroid cysts can also be seen in polynodular aneurysms, but usually in less than 10%). The smear is poor in cells but mostly small thyroid cysts. The smear is poor in cells but full of Hürthle cells. The smear is almost entirely benign, but there are few cells with scattered grooved nuclei. The slide contains many lymphocytes and plasma cells with some lymphocytes with atypical nuclei. Cellular abnormalities cannot be classified, eg few cells with large nuclei, enlarged nucleoli. 5.4 Group IV - Suspicious for follicular neoplasm The macroscopic and microscopic images of cystic carcinoma and benign cystic thyroid tumor can be identical; The malignancy of the tumor is determined only by the invasion of tumor cells into the capsule or blood vessels, which cannot be evaluated on cytological specimens.
Therefore, FNAC can only diagnose a suspected nodular lesion of the thyroid gland called a cystic thyroid nodule, but cannot differentiate between benign and malignant. Group IV patients with a risk of malignancy of 15-30%, will undergo a corresponding lobectomy.
5.5 Group V - Suspicious for malignancy accounts for about 2.4-7.9% of thyroid FNAC cases. The cytology specimen of patient
in this group still has normal follicular cells, but some cells have
features that are suspicious of thyroid cancer; Thus, the quantity is not enough to be classified in group VI. Particularly, cases of suspected follicular thyroid tumor or Hrthle cell tumor are not included in this group, but in group IV. Patients with group V have a risk of malignancy from 60-75%, will be operated with cryosection to decide whether to remove only 1 thyroid lobe or to remove the thyroid gland nearly completely.
Suspected papillary thyroid carcinoma Aspiration cytology containing honeycomb-shaped clusters of normal follicular cells; interspersed with a few cells with large oval nuclei, slightly pale, grooved but often do not create papillary structure.
In Hashimoto's thyroiditis and polygranulomatous thyroiditis, some Hürthle cells may have large oval and grooved nuclei, but no inclusions in the nucleus; Therefore, if nodules are seen, papillary thyroid carcinoma should be suspected. (Figure 12)
Suspect medullary thyroid carcinoma when on the slide there are several relatively discrete groups of cells with a high nuclear/cytoplasmic ratio, lateral nuclei, and a slightly salt-and-pepper appearance. The slide matrix may contain several small clusters of amorphous material, whether amyloid or colloid. Suspect thyroid lymphoma when the specimen contains a relatively uniform number of lymphocytes of relatively uniform size and atypical nuclei, in addition to clusters of normal follicular cells. Suspected malignancy, unspecified when the slide contains a few scattered cells, suspected malignancy but cannot be determined to be primary thyroid or metastatic. 5.6 Group VI - Malignant Thyroid diseases with cytological malignancy include papillary thyroid carcinoma, poorly differentiated thyroid carcinoma, undifferentiated thyroid carcinoma, medullary thyroid carcinoma, lymphoma and Carcinomas from elsewhere have metastasized to the thyroid gland. Group VI accounts for about 4-8% of thyroid FNAC cases, the vast majority of which are papillary thyroid carcinomas. Patients with group VI have a malignancy risk of 97-99% and will undergo a total thyroidectomy. Papillary thyroid carcinoma: Papillary thyroid carcinoma is the most common type of follicular cell carcinoma, accounting for 60-80% of primary thyroid cancers. The average age of disease is 40 years old, however, tumors can occur at any age, including children; Females are more susceptible to the disease than males. Fine-needle aspiration cytology has the following features: (Figures 4, 5)
Tumor cells form a 2-dimensional single-layer papillary structure or a 3-dimensional papillary structure containing a vascular axis; however, 3-dimensional papillae are relatively uncommon. Tumor cells have large oval nuclei, light colored superimposed on each other, nuclei have grooves and inclusion bodies. These nuclear features can be found relatively easily throughout the specimen. In addition, squamous tumor cells (with dense cytoplasm), polymorphonuclear macrophages (macrophage origin), zigzag solid colloids, and psammoma bodies (found in 4-20% of cases) can also be seen. papillary thyroid carcinoma).

Hình 4: Carcinôm tuyến giáp dạng nhú, tế bào u tạo thành nhú 1 lớp 2 chiều (A); hoặc nhú 3 chiều có trục liên kết mạch máu (mũi tên) (B).

Hình 5: Carcinôm tuyến giáp dạng nhú, tế bào có nhân lớn hình bầu dục, lợt mầu, chồng chất lên nhau và có rãnh (mũi tên) (A); một số nhân có thể vùi (mũi tên) (B).
Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical doctors, modern equipment and technology, but also stands out for its examination and consultation services. comprehensive and professional medical consultation and treatment; civilized, polite, safe and sterile medical examination and treatment space. Customers when choosing to perform tests here can be completely assured of the accuracy of test results.
Customers can directly go to Vinmec Health system nationwide to visit or contact the hotline here for support.
References: Textbook of Cytology of GPB Department, Pham Ngoc Thach Medical University, HCMC.
Bài viết này được viết cho người đọc tại Sài Gòn, Hà Nội, Hồ Chí Minh, Phú Quốc, Nha Trang, Hạ Long, Hải Phòng, Đà Nẵng.






