Slow-onset causes of wheezing
The article is written by Master, Doctor Ma Van Tham - Department of Pediatrics - Neonatology - Vinmec Phu Quoc International General Hospital.
Wheezing in infants and children < 5 years of age is very common. More than 30% of children under 3 years of age have at least one episode of wheezing, about 50% of children under 5 years of age have at least one episode of wheezing. About half of all children who develop wheezing before age 3 will not have a recurrence by age 6.
1. Structural Abnormalities
Structural abnormalities are an important cause of early-onset wheezing in the first months of life, including abnormalities of the bronchial tree and vascular annulus.
1.1. Abnormalities of the bronchial tree structure
Congenital tracheobronchial anomalies may present with abnormal breathing sounds in the early postpartum period. Wheezing can manifest after birth but is most often evident after 2 months of age. Wheezing may be monophonic, may become polyphonic on exertion, or be mixed with other noises when associated with an upper respiratory tract infection. Other symptoms that may be present include cough and stridor, depending on the location of the obstruction.
Evaluation of a patient with suspected tracheobronchial abnormalities should begin with routine chest x-ray. It often provides diagnostic information and excludes less likely diagnoses. It also provides preliminary information on cardiac shadow, pulmonary artery arch, and pulmonary perfusion status. Upper airway endoscopy may be necessary. If pulmonary aneurysm is suspected, contrast esophagography in combination with contrast-enhanced CT angiography or contrast-enhanced MRI should be performed.
Chest CT can also detect narrowing of central airways such as the trachea and main bronchi. However, bronchoscopy (during spontaneous breathing) is often required for an accurate diagnosis. Cartilage abnormalities can be identified by a decrease in airway diameter during expiration. Bronchoscopy can also be used to diagnose airway obstruction caused by internal or external airway compression, or by an abnormal vascular structure.
Evaluation of a patient with suspected tracheobronchial abnormalities should begin with routine chest x-ray. It often provides diagnostic information and excludes less likely diagnoses. It also provides preliminary information on cardiac shadow, pulmonary artery arch, and pulmonary perfusion status. Upper airway endoscopy may be necessary. If pulmonary aneurysm is suspected, contrast esophagography in combination with contrast-enhanced CT angiography or contrast-enhanced MRI should be performed.
Chest CT can also detect narrowing of central airways such as the trachea and main bronchi. However, bronchoscopy (during spontaneous breathing) is often required for an accurate diagnosis. Cartilage abnormalities can be identified by a decrease in airway diameter during expiration. Bronchoscopy can also be used to diagnose airway obstruction caused by internal or external airway compression, or by an abnormal vascular structure.
1.2. Cardiovascular disease
Cardiovascular conditions that can cause wheezing include:
Cardiovascular conditions that result in pulmonary artery dilation or increased left heart chamber load can compress the large airways and cause wheezing. In addition to narrowing of the bronchi due to dilatation of the main pulmonary arteries, possible narrowing of the airways due to aberrant pulmonary artery branches has been reported in patients with cardiomegaly (those branches are the systemic circulation). expand the lungs causing pressure on the airways).
Left heart failure or pulmonary venous stenosis causes pulmonary vascular bed dilation, leading to pulmonary congestion, increased airway resistance, wheezing. Bronchial hyperreactivity has also been reported in patients with congenital heart disease. One hypothesis is that increased pulmonary venous pressure may cause pulmonary venous hypertrophy, increased pulmonary vasoconstriction, and as a final event, the release of vasoactive substances that influence both response and response. vasoconstriction and bronchospasm, leading to a state of "pseudo-asthma". In some young children with pulmonary venous return obstruction, cardiac abnormalities including cardiac enlargement and heart murmur may not be found. Wheezing has been reported as the only symptom present in cases of triatrial heart disease.
Loops or slings can cause major airway obstruction and can lead to wheezing or stridor. These include complete loops (eg, double aorta) and incomplete loops (eg, pulmonary sling). Right pneumothorax may be noted in patients with pulmonary artery sling.
Cardiovascular conditions that result in pulmonary artery dilation or increased left heart chamber load can compress the large airways and cause wheezing. In addition to narrowing of the bronchi due to dilatation of the main pulmonary arteries, possible narrowing of the airways due to aberrant pulmonary artery branches has been reported in patients with cardiomegaly (those branches are the systemic circulation). expand the lungs causing pressure on the airways).
Left heart failure or pulmonary venous stenosis causes pulmonary vascular bed dilation, leading to pulmonary congestion, increased airway resistance, wheezing. Bronchial hyperreactivity has also been reported in patients with congenital heart disease. One hypothesis is that increased pulmonary venous pressure may cause pulmonary venous hypertrophy, increased pulmonary vasoconstriction, and as a final event, the release of vasoactive substances that influence both response and response. vasoconstriction and bronchospasm, leading to a state of "pseudo-asthma". In some young children with pulmonary venous return obstruction, cardiac abnormalities including cardiac enlargement and heart murmur may not be found. Wheezing has been reported as the only symptom present in cases of triatrial heart disease.
Loops or slings can cause major airway obstruction and can lead to wheezing or stridor. These include complete loops (eg, double aorta) and incomplete loops (eg, pulmonary sling). Right pneumothorax may be noted in patients with pulmonary artery sling.

Nguyên nhân thở khò khè do các bất thường động mạch từ hoàn toàn đến không hoàn toàn (a–Động mạch chủ đôi e;- Sling động mạch phổi)
Signs and symptoms of vascular abnormalities usually appear early in life. Bidirectional stridor is the most common finding in these patients, but wheezing, respiratory distress, recurrent respiratory tract infections, and apnea may also occur in these patients. Patients may also have symptoms due to esophageal compression by vascular structures, including difficulty feeding and vomiting.
Physical examination revealed signs of rough, bipartite wheezing, which was relieved with neck relaxation to reduce airway compression.
Diagnostic evaluation of children with suspected loops or slings:
Routine chest radiograph, which is abnormal in most cases. There is almost always a dominant right aortic loop that can cause tracheal stenosis, tracheal deviation. Signs may include tracheal deviation, tracheal opacity, tracheal stenosis, or all of the above. The next step in the diagnostic workup may include an MRA, or contrast-enhanced CT angiogram. Bronchoscopy is not required in all suspected patients or to confirm the diagnosis. It is useful in determining the location and severity of airway obstruction and in evaluating airway cartilage abnormalities. However, it cannot define the anatomy of an annulus, and carries the risk of causing airway edema, which can worsen tracheal obstruction.
Physical examination revealed signs of rough, bipartite wheezing, which was relieved with neck relaxation to reduce airway compression.
Diagnostic evaluation of children with suspected loops or slings:
Routine chest radiograph, which is abnormal in most cases. There is almost always a dominant right aortic loop that can cause tracheal stenosis, tracheal deviation. Signs may include tracheal deviation, tracheal opacity, tracheal stenosis, or all of the above. The next step in the diagnostic workup may include an MRA, or contrast-enhanced CT angiogram. Bronchoscopy is not required in all suspected patients or to confirm the diagnosis. It is useful in determining the location and severity of airway obstruction and in evaluating airway cartilage abnormalities. However, it cannot define the anatomy of an annulus, and carries the risk of causing airway edema, which can worsen tracheal obstruction.
1.3. Abnormal mass of mediastinum
Mediastinal abnormalities including tumors, thymus, lymph nodes, and bronchial cysts can compress the airways causing chronic cough and persistent or recurrent wheezing.
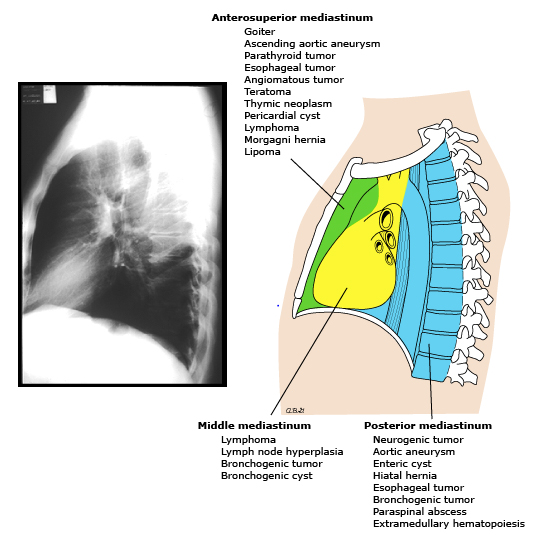
Nguyên nhân thở khò khè do các khối bất thường trung thất
Routine chest radiographs revealed an abnormal mass in the mediastinum in most cases. However, bronchial cysts may not be evident on chest radiographs or may lead to localized air retention resembling congenital lobar emphysema.
CT, MRI, mediastinal ultrasonography, contrast esophagography, and bronchoscopy may be indicated in cases of need.
CT, MRI, mediastinal ultrasonography, contrast esophagography, and bronchoscopy may be indicated in cases of need.
2. Abnormal function
2.1. Inhalation syndrome
Aspiration syndromes are important and often unrecognized causes of wheezing in young children. In many cases, these patients are misdiagnosed with uncontrolled asthma. Respiratory distress syndrome is associated with a variety of structural and functional disorders. These disorders can be divided into four main categories:
Foreign body in the airways: As stated above. However, with a neglected airway foreign body, symptoms are usually persistent cough, wheezing, and recurrent or persistent pneumonia. Gastroesophageal reflux disease (GERD): Gastroesophageal reflux disease (GER) is rarely associated with aspiration of large amounts of gastric juice. However, long-term inhalation of small amounts of gastric juice can cause mucosal edema and mucositis, which can lead to chronic coughing and wheezing. Bottle-fed infants in bed are at increased risk of wheezing and developing asthma during the first five years of life, possibly due to prolonged aspiration of gastric juices. Children with GERD do not always have typical reflux symptoms, such as heartburn or vomiting, but may present more subtle, including nocturnal symptoms, hoarseness, or recurrent laryngitis. to act. Swallowing disorders associated with nerve or muscular dysfunction of the pharynx and/or larynx can lead to weakness and impaired swallowing ability, incomplete closure of the epiglottis, decreased cough reflexes, and aspiration recurrent epistaxis. Anatomical abnormalities, such as laryngeal clefts and vocal cord paralysis, can also cause swallowing dysfunction leading to aspiration syndrome. The first step in making a diagnosis is to observe the baby while nursing: The baby has trouble sucking or swallowing, is tired, loses interest, has rapid breathing, or stops breathing. The classic symptom of coughing with food may be absent because of decreased cough reflex due to irritation at receptors in the larynx and trachea. Video-enhanced esophagography, combined with swallowing evaluation by a linguist, can be useful for both diagnostic and therapeutic purposes. Fissures between the tracheobronchial tree and other anatomical structures can cause wheezing. Tracheoesophageal fistula, the most common in this group. Some infants with H-type tracheoesophageal fistula are not immediately diagnosed in the postpartum period. These children may have chronic cough and recurrent pneumonia as well as wheezing. Symptoms such as coughing and choking increase with eating. Chest radiograph may show chronic infiltrates. However, bronchoscopy and/or esophagoscopy is required to confirm this diagnosis.
Foreign body in the airways: As stated above. However, with a neglected airway foreign body, symptoms are usually persistent cough, wheezing, and recurrent or persistent pneumonia. Gastroesophageal reflux disease (GERD): Gastroesophageal reflux disease (GER) is rarely associated with aspiration of large amounts of gastric juice. However, long-term inhalation of small amounts of gastric juice can cause mucosal edema and mucositis, which can lead to chronic coughing and wheezing. Bottle-fed infants in bed are at increased risk of wheezing and developing asthma during the first five years of life, possibly due to prolonged aspiration of gastric juices. Children with GERD do not always have typical reflux symptoms, such as heartburn or vomiting, but may present more subtle, including nocturnal symptoms, hoarseness, or recurrent laryngitis. to act. Swallowing disorders associated with nerve or muscular dysfunction of the pharynx and/or larynx can lead to weakness and impaired swallowing ability, incomplete closure of the epiglottis, decreased cough reflexes, and aspiration recurrent epistaxis. Anatomical abnormalities, such as laryngeal clefts and vocal cord paralysis, can also cause swallowing dysfunction leading to aspiration syndrome. The first step in making a diagnosis is to observe the baby while nursing: The baby has trouble sucking or swallowing, is tired, loses interest, has rapid breathing, or stops breathing. The classic symptom of coughing with food may be absent because of decreased cough reflex due to irritation at receptors in the larynx and trachea. Video-enhanced esophagography, combined with swallowing evaluation by a linguist, can be useful for both diagnostic and therapeutic purposes. Fissures between the tracheobronchial tree and other anatomical structures can cause wheezing. Tracheoesophageal fistula, the most common in this group. Some infants with H-type tracheoesophageal fistula are not immediately diagnosed in the postpartum period. These children may have chronic cough and recurrent pneumonia as well as wheezing. Symptoms such as coughing and choking increase with eating. Chest radiograph may show chronic infiltrates. However, bronchoscopy and/or esophagoscopy is required to confirm this diagnosis.

Nguyên nhân thở khò khè do các type rò khí thực quản
2.2. Immune abnormalities
Recurrent lower respiratory tract infections may present with episodes of wheezing. These conditions can lead to bronchiectasis, permanent parenchymal destruction, and chronic lung disease if not known or inadequately treated. Immune deficiency syndromes, particularly those associated with immunoglobulin G (IgG) and/or immunoglobulin A (IgA) deficiencies, are the most common abnormalities that can cause respiratory tract infections. recurrent inhalation. Both the upper and lower airways can be affected and can lead to otitis media, pharyngitis, or pneumonia. Complement deficiencies, T-cell abnormalities, and defects in leukocyte activity can lead to upper and lower respiratory tract infections, but are less common.
PCD (respiratory hairy epithelial structural and functional abnormalities) is a rare disease that can present with chronic cough and wheezing in children. This diagnosis should be considered in patients with severe upper respiratory tract infections, recurrent otitis media, and chronic sinusitis.
PCD (respiratory hairy epithelial structural and functional abnormalities) is a rare disease that can present with chronic cough and wheezing in children. This diagnosis should be considered in patients with severe upper respiratory tract infections, recurrent otitis media, and chronic sinusitis.
2.3. Cystic fibrosis
Cystic fibrosis, also known as viscous mucus disease, is an inherited disorder that affects the respiratory tract, digestive tract, and reproductive system involving the production of abnormally thick mucus lining the lungs and can lead to fatal lung infection. The disease can also cause various blockages of the pancreas, which interfere with digestion. Children must carry both disease genes from their parents to manifest the disease. The incidence is different around the world. In Europe, the rate is 1 in 2,000 – 3,000 live births. In the United States, the reported incidence is one in 3,500 live births. The severity of cystic fibrosis varies greatly from person to person regardless of age, severity being determined primarily by the extent to which the lungs are affected.
Inflammation and infection cause damage and structural changes to the lungs. Symptoms occur when bacteria that normally live in mucus grow out of control and cause pneumonia. Staphylococcus aureus, Haemophilus influenzae, and Pseudomonas aeruginosa are the three most common organisms that cause lung infections in patients with cystic fibrosis.
Diagnosis is based on family history, clinical symptoms, and sweat testing showing a chlorine ratio ≥ 60 mmol/L with sweat > 100 mg, made by chromatography. If in doubt, a second test or genetic testing should be performed.
Inflammation and infection cause damage and structural changes to the lungs. Symptoms occur when bacteria that normally live in mucus grow out of control and cause pneumonia. Staphylococcus aureus, Haemophilus influenzae, and Pseudomonas aeruginosa are the three most common organisms that cause lung infections in patients with cystic fibrosis.
Diagnosis is based on family history, clinical symptoms, and sweat testing showing a chlorine ratio ≥ 60 mmol/L with sweat > 100 mg, made by chromatography. If in doubt, a second test or genetic testing should be performed.
2.4. Bronchopulmonary dysplasia
Bronchopulmonary dysplasia (BPD), also known as chronic lung disease or chronic lung disease of infancy, is an important cause of respiratory illness in premature infants, especially those born with weight less than 1250 g. The causes of BPD are manifold. Most patients had a history of neonatal respiratory distress syndrome.
The diagnosis of BPD is mainly based on the history of preterm birth and the need for supplemental oxygen beyond 36 weeks gestation. Chest radiograph shows diffuse lesions, which may be diffuse opacities, reflecting inflammation and/or pulmonary edema. Lung capacity is normal or low, and there may be areas of atelectasis alternating with areas of air retention.
The diagnosis of BPD is mainly based on the history of preterm birth and the need for supplemental oxygen beyond 36 weeks gestation. Chest radiograph shows diffuse lesions, which may be diffuse opacities, reflecting inflammation and/or pulmonary edema. Lung capacity is normal or low, and there may be areas of atelectasis alternating with areas of air retention.
2.5. Paradoxical mobility of the vocal cords
This is a condition that affects older children, often teenagers, and adults. In a normal larynx, the vocal cords actually open during inhalation and exhalation and close during speaking, swallowing, and coughing. In contrast, paradoxical vocal cord motion (PVCM) or vocal cord dysfunction is an inappropriate closure of the vocal cords during inspiration and opening during expiration. Functional airway obstruction arising from vocal cord closure during inspiration causes significant respiratory distress and signs of stridor or wheezing.
PVCM is associated with many psychosocial disorders; However, it is not considered a form of self-aggrandizement, as the patient did not intentionally induce the condition. It is also linked to stress, exercise, airway surgery and nerve damage, GERD, and inhalation of airway irritants. PVCM may be associated with underlying asthma, although it is frequently misdiagnosed as asthma. In these patients, an incorrect diagnosis has led to overuse of drugs, including systemic glucocorticoids, repeated emergency visits, frequent hospitalizations, intubation, and even tracheostomy. .
Clinical manifestations may range from pseudo-asthmatic signs to upper airway obstruction. Wheezing or stridor should resolve completely while the patient is asleep or shortly after intubation or tracheostomy. Patients may complain of dyspnea, sore throat, feeling of choking, difficulty speaking, and coughing.
Pulmonary function testing is usually normal, although flow–volume loops on spirometry may show flattening of the inspiratory loop (bottom figure), consistent with upper airway obstruction. Oxygen saturation is often higher than 94%, even during periods of significant respiratory failure. Observation of the vocal cords when the patient is symptomatic using a fiberoptic laryngoscope can confirm the diagnosis.
PVCM is associated with many psychosocial disorders; However, it is not considered a form of self-aggrandizement, as the patient did not intentionally induce the condition. It is also linked to stress, exercise, airway surgery and nerve damage, GERD, and inhalation of airway irritants. PVCM may be associated with underlying asthma, although it is frequently misdiagnosed as asthma. In these patients, an incorrect diagnosis has led to overuse of drugs, including systemic glucocorticoids, repeated emergency visits, frequent hospitalizations, intubation, and even tracheostomy. .
Clinical manifestations may range from pseudo-asthmatic signs to upper airway obstruction. Wheezing or stridor should resolve completely while the patient is asleep or shortly after intubation or tracheostomy. Patients may complain of dyspnea, sore throat, feeling of choking, difficulty speaking, and coughing.
Pulmonary function testing is usually normal, although flow–volume loops on spirometry may show flattening of the inspiratory loop (bottom figure), consistent with upper airway obstruction. Oxygen saturation is often higher than 94%, even during periods of significant respiratory failure. Observation of the vocal cords when the patient is symptomatic using a fiberoptic laryngoscope can confirm the diagnosis.

Thăm dò chức năng hô hấp ( A: Bình thường; B: Tắc nghẽn đường hô hấp trên ngoài lồng ngực; C: Tắc nghẽn đường hô hấp trên trong lồng ngực; D: Hỗn hợp B và C; E: Tắc nghẽn đường hô hấp dưới)
2.6. Organized Obstructive Bronchiolitis
Organizing obstructive bronchiolitis (BO) (or obstructive bronchiolitis in some documents) is a rare disease caused by damage to the lower airway epithelium leading to obstruction and destruction of the airways. breathe far. BO can occur after a chemical, infectious, or immune injury but can be spontaneous. Damage to the bronchioles following viral infection is one of the most common causes of BO. Adenovirus is the virus capable of causing BO, but other pathogens, including influenza, measles, and mycoplasma, have also been detected in association with BO. BO is often seen in children who have undergone a stem cell transplant.
Clinical symptoms include tachypnea, dyspnea, persistent cough, and wheezing unresponsive to bronchodilator therapy. Hypoxia occurs in more severe cases, at rest or exertion and or during sleep. Examination revealed diffuse rales and wheezing in both lungs. Pulmonary function measurements revealed airway obstruction without significant response to bronchodilators.
Clinical symptoms include tachypnea, dyspnea, persistent cough, and wheezing unresponsive to bronchodilator therapy. Hypoxia occurs in more severe cases, at rest or exertion and or during sleep. Examination revealed diffuse rales and wheezing in both lungs. Pulmonary function measurements revealed airway obstruction without significant response to bronchodilators.
2.7. Interstitial lung disease
Interstitial lung disease (ILD), also known as interstitial pneumonia, is a group of rare disorders that involve the lung parenchyma and interfere with gas exchange. Affected children often present with progressive dyspnea, which worsens with exertion, and rarely cyanosis. Wheezing is reported in about half of children with ILD, although it is rarely detected on physical examination. The occurrence of rales, mainly during inspiration, is common in most ILDs. Clubbing is a late manifestation of advanced fibrosis of the lung. Pulmonary function measurements often show a restrictive pattern, with reduced gas diffusion (lung diffusing capacity for carbon monoxide [DLCO]).
Để đặt lịch khám tại viện, Quý khách vui lòng bấm số HOTLINE hoặc đặt lịch trực tiếp TẠI ĐÂY. Tải và đặt lịch khám tự động trên ứng dụng MyVinmec để quản lý, theo dõi lịch và đặt hẹn mọi lúc mọi nơi ngay trên ứng dụng.






