This is an automatically translated article.
Acute respiratory distress syndrome is a medical condition caused by acute damage to the alveolar capillary membranes in the lungs of various etiologies, leading to progressive respiratory failure and unresponsiveness to high doses of oxygen. .
1. What is progressive acute respiratory distress syndrome?
Acute respiratory distress syndrome (ARDS) is an acute condition in which damage to the alveolar capillary membranes, due to a variety of intrapulmonary and extrapulmonary causes, causes progressive respiratory failure that is unresponsive to high doses of oxygen. normal high. ARDS was first described by Ashbaugh et al in 1967.
In 2011, a conference of leading respiratory experts came up with the BERLIN definition of ARDS for clinical diagnosis and evaluation:
Duration: Within 1 week of onset of risk factors or worsening of respiratory distress symptoms. X-ray or CT image: Appears diffuse opacities in both lungs, unexplained cause is pleural effusion, atelectasis or tumor in lung Origin of alveolar edema: Respiratory failure Progressive respiratory failure not due to heart failure or fluid overload (recommended echocardiographic assessment). Blood oxygenation level: Mild: 200 mmHg < PaO2/FIO2 < 300 mmHg with PEEP or CPAP ≥ 5 cmH2O; Moderate: 100 mmHg < PaO2/FIO2 < 200 mmHg with PEEP ≥ 5 cmH2O; Severe: PaO2/FIO2 < 100 mmHg with PEEP ≥ 5 cmH2O.

Hội chứng suy hô hấp cấp tiến triển tình trạng tổn thương cấp tính màng phế nang mao mạch
2. Causes of progressive acute respiratory distress syndrome
2.1 Pulmonary causes
Severe pneumonia: Pneumonia is the most common cause. The causative agent of pneumonia can be bacteria (pneumococcus, streptococcus, H. influenzae...) or viruses (influenza A H5N1, SARS...); Asphyxiation: With the main mechanism being damage to the alveolar surfactant membrane; Gastroesophageal reflux: Acid reflux from the stomach will cause extensive lung damage with atelectasis, this cause is common in comatose or drunk patients; Injecting, snorting heroin or using narcotic drugs (cocaine, amphetamine...); Direct trauma to the chest causes contusion, lung damage.
2.2 Extrapulmonary causes
Severe infections such as sepsis or septic shock can also cause acute respiratory failure. Bulk blood transfusion (>15 units). Severe acute pancreatitis.

Viêm tụy cấp nặng là nguyên nhân ngoài phổi gây hội chứng suy hô hấp cấp tiến triển
3. Diagnostic guidelines for acute respiratory distress syndrome
3.1 Clinical Manifestations
Rapidly progressive respiratory failure: rapid onset within 6–72 hours; Patients have difficulty breathing, rapid breathing, contraction of accessory respiratory muscles such as intercostal muscles, depression of the sternum, chest indrawing and tissue hypoxia such as cyanosis of the lips and extremities...; Appears diffuse rattles throughout the 2 lungs; Tachycardia, sweating, patient agitation; Signs suggestive of the cause of acute respiratory distress syndrome such as fever, rash, coagulopathy...
3.2 Test results
Blood gas test: PaO2 decreased, often with decreased CO2; Chest X-ray: diffuse infiltrates of 2 lungs; Chest computed tomography: diffuse infiltrative lesions of 2 lungs.
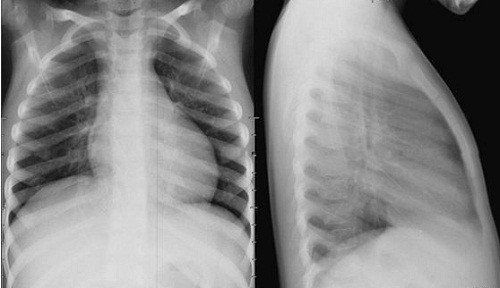
X quang phổi giúp chẩn đoán hội chứng suy hô hấp cấp tiến triển
3.3 Differential diagnosis
Acute hemodynamic pulmonary edema: due to acute left heart failure or acute fluid overload. Diffuse alveolar hemorrhage: Acute respiratory failure is accompanied by rapid blood loss and the patient coughs up bloody sputum or bronchoscopy shows blood.
4. Guidelines for the treatment of acute respiratory distress syndrome
4.1 General principles of treatment
Support patient breathing with artificial ventilation with lung protection strategy. Identify and treat causes of progressive respiratory failure.
4.2 Artificial ventilation
Give patients invasive (through endotracheal) or non-invasive ventilation (CPAP or BiPAP)
Targets to be achieved
Blood oxygenation level: arterial blood gas with PaO2 55 - 80 mmHg or SpO2 reached from 88 - 95%, arterial blood pH: 7.25 - 7.45; Plateau pressure (Pplateau) ≤ 30 cmH2O; Maintain the patient's breathing rate from 14 to 35 times/minute to ensure that the minute ventilation reaches 6 - 8 liters/min; Hypercoaemia is acceptable as long as the blood oxygenation target is maintained and the plateau pressure is below 30 cmH2O of water. If mechanical ventilation in patients with advanced respiratory failure does not meet the goals and technical conditions allow, the patient should use cardiopulmonary bypass (ECMO) with mechanical ventilation to avoid collapse. lung.

Sử dụng kỹ thuật tim phổi nhân tạo kèm thở máy để tránh xẹp phổi
4.3 Correction of acid-base balance disorder
If blood pH is between 7.15 – 7.25: Increase respiratory rate to reach target pH. If pH < 7.15: Increase respiratory rate to 35 breaths/min, consider intravenous bicarbonate solution.
4.4 Use of sedatives – muscle relaxants
In order to effectively treat acute respiratory distress syndrome, the patient must be completely mechanically ventilated, so it is recommended to use sedatives or add drugs. However, the use of these drugs needs to be appropriate for each patient, need to reduce the dose and stop at the right time when the disease improves to stop the ventilator in time and stop the machine as soon as possible.
4.5 Ensure hemodynamics and balance water demand
Monitor the patient's weight every day to assess the amount of fluid in and out and make sure not to overload the fluid. If fluid overload occurs, and the patient gains weight, intravenous furosemide diuretics should be administered at an appropriate dose to reduce fluid loss in the urine. Preferably rely on CVP (maintain central venous pressure between 6 and 8 cmH2O).4.6 Other treatments
Control blood sugar: Maintain blood glucose from 6-10 mmol/L with Insulin; Anti-infective antibiotics: Use antibiotics immediately after mechanical ventilation, adjust according to the antibiotic chart (if any) and gradually de-escalate; Prophylaxis of thromboembolism: use prophylactic dose heparin; Prophylaxis of gastrointestinal bleeding due to peptic ulcer: the patient lying motionless for a long time can affect the stomach, causing ulceration and possible gastrointestinal bleeding. Prophylaxis with proton pump inhibitors; Ensure adequate blood volume (Hb > 8 grams/liter).

Kiểm soát đường huyết giúp điều trị hội chứng suy hô hấp cấp tiến triển
5. Complications of acute respiratory distress syndrome
Complications from treatment (especially mechanical ventilation):
Alveolar trauma causing alveolar rupture due to pressure overload. Hospital pneumonia. Other complications:
Psychosis; Deep vein thrombosis: prophylaxis with heparin; Gastroesophageal ulcers: prophylaxis with proton pump inhibitors; Malnutrition: Feeding through the stomach or through the vein; Catheter infections: prophylactic antibiotics. Acute respiratory distress syndrome has a high mortality rate, so as soon as there are signs of the disease, you should go to a reputable medical facility for examination and treatment. To detect the disease early, you should have regular check-ups.
Currently, Vinmec International General Hospital has general health checkup packages suitable for each age, gender and individual needs of customers with a reasonable price policy, including:
Health checkup package Diamond Health Checkup Package Vip General Health Checkup Package Special General Health Checkup Package Comprehensive General Health Checkup Package Standard General Health Checkup Package Patient's examination results will be returned to your home. After receiving the results of the general health examination, if you detect diseases that require intensive examination and treatment, you can use services from other specialties at the Hospital with quality treatment and services. outstanding customer service.
To register for examination and treatment at Vinmec International General Hospital, you can contact the nationwide Vinmec Health System Hotline, or register online HERE.