This article is professionally reviewed by Nguyen Hoang Phuong Khanh, MSc, BPharm - Clinical Pharmacist - Pharmacy Department - Vinmec Central Park International General Hospital.
With the advent of antibiotics, the medical approach to treating infectious diseases has entered a new era; thanks to antibiotics, millions of individuals have been saved from dangerous infections. So, what are antibiotics? What is the mechanism of action of antibiotics?
1. Definition of Antibiotics
Alexander Fleming (1881 – 1955) was a physician, biologist, and pharmacologist from Scotland. He is regarded as the pioneer in the use of antibiotics in medicine.
Antibiotics are antimicrobial substances produced by various microbial species or synthesized chemically, which inhibit the growth and development or kill other microorganisms.
2. Classification of Antibiotics
There are several methods to classify antibiotics; however, common classifications include categorization by spectrum of activity and by mechanism of action.
2.1 Classification by Spectrum of Activity
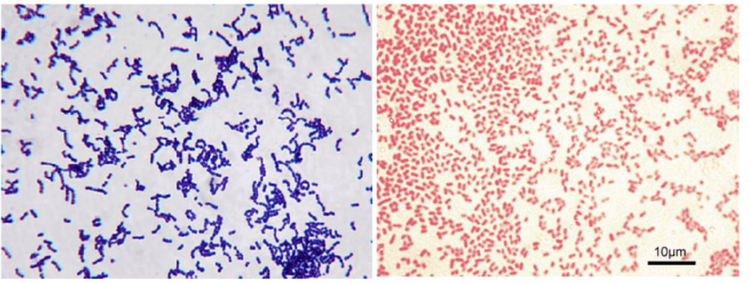
Due to the specific mechanisms of action of each antibiotic type, each group acts on a limited number of bacterial strains. This limitation is referred to as the antibacterial spectrum of the antibiotic.
- Narrow-spectrum antibiotics (selective antibiotics): Antibiotics that are effective against one or a limited number of specific microorganisms. For example, isoniazid is effective solely against Mycobacterium tuberculosis.
- Broad-spectrum antibiotics: Antibiotics that have activity against numerous types of bacteria, including both Gram-negative and Gram-positive bacteria, such as the quinolone, macrolide, and carbapenem groups.
Inappropriate use of broad-spectrum antibiotics may disrupt the resident microbiota of the body and lead to secondary infections (such as Clostridium difficile infections) following antibiotic administration.
2.2 Classification by Chemical Structure
Beta-lactam Group: Comprises antibiotics with a chemical structure containing a beta-lactam ring, which is further divided into four groups:
- Penicillin: Derivatives of 6-aminopenicillanic acid. This includes: benzylpenicillin, methicillin, amoxicillin, piperacillin, etc. Penicillin exhibits activity against both Gram-positive and Gram-negative organisms. However, due to bacterial resistance mechanisms, such as the production of beta-lactamase enzymes, certain antibiotics are supplemented with beta-lactamase inhibitors to enhance their antibacterial efficacy, such as amoxicillin/clavulanic acid and piperacillin/tazobactam.
- Cephalosporin: Composed of a beta-lactam ring and a dihydrothiazine ring. Modifications of substituent groups on the ring result in changes to the properties and biological activities of the antibiotic. Cephalosporins are categorized into four generations.
- First Generation: Primarily effective against Gram-positive bacteria: cefazolin, cefalexin
- Second Generation: Broader activity against Gram-negative bacteria: cefuroxime, cefamandole, cefaclor, along with activity against anaerobic bacteria Bacteroides fragilis: cefotetan, cefoxitin
- Third Generation: Potent against Gram-negative organisms: cefotaxime, ceftriaxone, ceftazidime, cefixime.
- Fourth Generation: Broad spectrum on both Gram-positive and Gram-negative organisms, including Pseudomonas: cefepime.
- Fifth Generation: Includes activity against MRSA (Methicillin-resistant Staphylococcus aureus): ceftaroline
- Carbapenem: These antibiotics have a high affinity for penicillin-binding proteins (PBPs) in both Gram-positive and Gram-negative bacteria, combined with a structure that is resistant to degradation by beta-lactamase enzymes, making this the broadest spectrum subgroup within the beta-lactams, exemplified by meropenem, imipenem-cilastatin, and ertapenem. This group of antibiotics is considered a "last resort," utilized exclusively in severe infections or cases of multidrug resistance.
- Monobactam: This class encompasses antibiotics containing only a beta-lactam ring, primarily effective against Gram-negative bacteria: Aztreonam.
Aminoglycoside Group (amikacin, tobramycin, gentamicin): Characterized by a chemical structure that contains a sugar moiety (ose) and an amino functional group, hence the designation of aminoglycosides. These antibiotics are effective against Gram-negative bacteria, with some activity against Gram-positive bacteria (gentamicin).

Macrolide Group: Isolated from Streptomyces. Commonly encountered active substances include erythromycin, clarithromycin, and azithromycin. This group of antibiotics exhibits activity against Gram-positive, Gram-negative, and atypical bacteria.
Lincosamide Group: This group includes two antibiotics, lincomycin and clindamycin. Clindamycin primarily targets Gram-positive bacteria and anaerobes.
Quinolone Group: These are completely synthetic antibiotics. First generation is represented by nalidixic acid, with subsequent generations modified by the addition of fluorine, hence the name fluoroquinolones. Examples include ciprofloxacin, levofloxacin, and moxifloxacin. This group exhibits potent activity against Gram-negative bacteria such as Enterobacteriaceae, Haemophilus spp., and Neisseria spp. Additionally, ciprofloxacin and levofloxacin demonstrate activity against Pseudomonas aeruginosa.
Glycopeptide Group (Vancomycin, Teicoplanin): This group consists of semisynthetic antibiotics with activity against Gram-positive bacteria, including various drug-resistant strains. Monitoring drug concentrations in the bloodstream is essential during administration to ensure therapeutic efficacy and minimize nephrotoxicity.
Other Groups:
Oxazolidone (linezolid): A completely synthetic antibiotic, exhibiting potent activity against Gram-positive bacteria such as Staphylococcus and Streptococcus. Furthermore, this drug demonstrates efficacy against multidrug-resistant Gram-positive bacteria like MRSA and VRE.
Chloramphenicol (chloramphenicol, thiamphenicol): Due to extended use, a high rate of drug resistance has developed. Additionally, these agents exhibit severe toxicity on hematopoietic systems, causing aplastic anemia, which has resulted in decreased clinical utilization.
Tetracycline (tetracycline, doxycycline, minocycline): These antibiotics possess a four six-membered ring structure, derived from Streptomyces aureofaciens or semi-synthetic processes. They have a broad spectrum of activity against Gram-positive, Gram-negative bacteria, and intracellular pathogens. Notably, these should not be administered to young children, as they bind strongly to bones and teeth, resulting in developmental delays, dental damage, and discoloration.
- Nitro-imidazole: These antibiotics are chemically synthesized: metronidazole, tinidazole. They exhibit activity against protozoa and anaerobes such as Bacteroides, Clostridium difficile, and Helicobacter pylori.
- Sulfonamide: Exhibiting bacteriostatic effects, these agents are not to be used as monotherapy. They have activity against Gram-positive, Gram-negative bacteria, Actinomyces, Chlamydia, Plasmodium, and Toxoplasma.
- Trimethoprim: Frequently combined with sulfonamide for the treatment of Gram-positive and Gram-negative infections, including those caused by multidrug-resistant organisms such as Acinetobacter, Burkholderia cepacia, and Stenotrophomonas maltophilia.
- Polymyxin (Polymyxin B, Colistin): This antibiotic is synthesized from Bacillus polymyxa. Following the introduction of aminoglycosides, polymyxins have seen decreased utilization due to high nephrotoxicity. Nevertheless, in light of the rising incidence of multidrug-resistant Gram-negative bacteria, polymyxins have been reintroduced for treating Acinetobacter spp. and Pseudomonas spp.
Anti-tuberculosis Antibiotics: rifampicin, isoniazid, pyrazinamide, ethambutol.
3. Mechanism of Action of Antibiotics
3.1 Inhibition of Bacterial Cell Wall Synthesis
- In Gram-negative bacteria:
The beta-lactam group enters the cell through porin channels in the outer membrane of the bacterial cell and binds to Penicillin Binding Proteins (PBPs), which are enzymes involved in the cross-linking of peptidoglycan to form the bacterial cell wall.
- In Gram-positive bacteria:
Gram-positive bacteria lack an outer membrane, thus beta-lactam acts directly on PBPs. The Glycopeptide group (e.g., Vancomycin) binds to D-alanyl-D-alanine, thereby affecting the peptidoglycan synthesis process.
3.2 Disruption of the Cytoplasmic Membrane
The cytoplasmic membrane primarily functions as a selective permeability barrier for substances. When antibiotics interact with the membrane, they alter its selective permeability, leading to the efflux of intracellular ions and an influx of external water, which ultimately results in cell death.
For example: Polymyxin B and colistin bind to the cell membrane of Gram-negative bacteria.
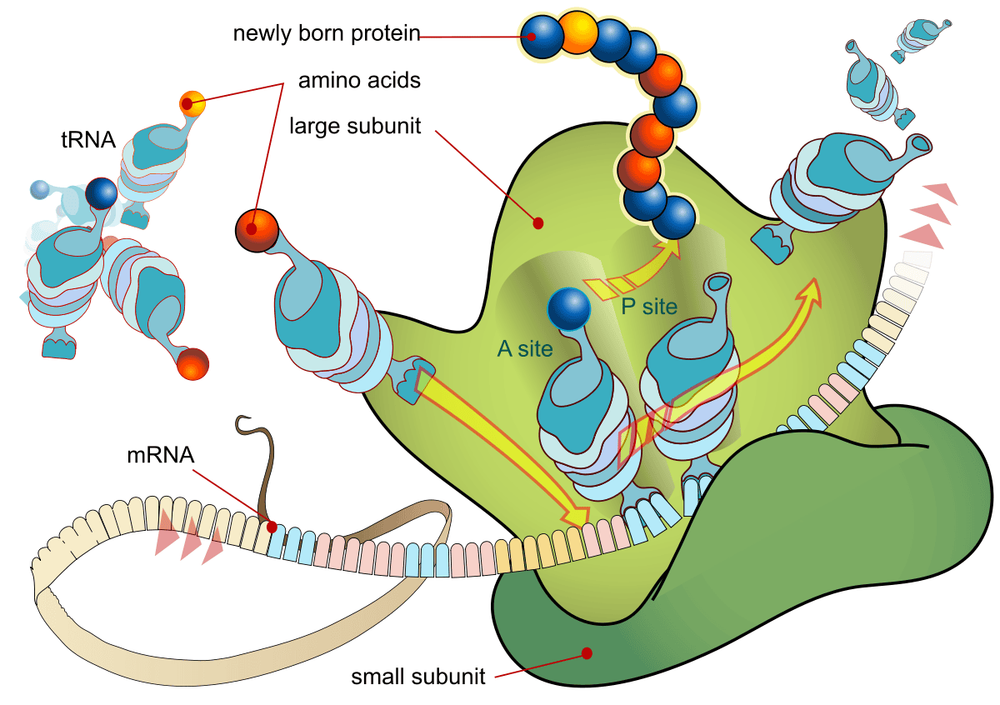
3.3 Inhibition of Protein Synthesis
- Tetracycline: binds to the 30S ribosomal subunit, preventing tRNA from binding to the mRNA-ribosome complex; it acts as a bacteriostatic agent.
- Aminoglycosides: bind to the 30S ribosomal subunit, inhibiting mRNA transcription while also causing misreading of mRNA; these are bactericidal antibiotics.
- Macrolides and lincosamides: bind to the 50S ribosomal subunit, terminating the development of the protein chain; they are bacteriostatic agents.
- Chlorpheniramine: binds to the 50S ribosomal subunit and inhibits the binding of amino acids to form the protein chain; it acts as a bacteriostatic antibiotic.
- Linezolid: binds to 23S ribosomal RNA of the 50S ribosomal subunit, inhibiting the formation of the 70S ribosomal complex necessary for protein synthesis; it is a bacteriostatic agent.
3.4 Inhibition of Nucleic Acid Synthesis
- Quinolones: target DNA gyrase and topoisomerase IV enzymes, affecting DNA replication.
- Rifampicin: binds to DNA-dependent RNA polymerase, inhibiting RNA synthesis in bacterial cells.
3.5 Inhibition of Folate Synthesis
- Sulfonamides: agents with a structure similar to para-aminobenzoic acid (PABA), competitively inhibit PABA, which is involved in the folic acid metabolic process (a precursor necessary for nucleic acid synthesis), thus acting as bacteriostatic agents.
- Trimethoprim: inhibits the enzyme dihydrofolate reductase, thereby affecting folic acid synthesis, with bacteriostatic activity.
Each antibiotic exhibits a distinct mechanism of action that impacts the growth and development of bacteria. Antibiotic combination therapy is often employed based on the site of action to enhance synergistic efficacy among antibiotics.
When selecting antibiotics for patient treatment, physicians consider the infection status, risk of multidrug-resistant bacteria, the location of the infection source, the antimicrobial spectrum of the antibiotics, and the permeability of the antibiotics into the infected tissue.
At Vinmec, a full range of antibiotics from the mentioned groups is readily available, ensuring quality and effective treatment of infections. Furthermore, the hospital has implemented an antibiotic stewardship program since 2017, involving close collaboration between physicians and clinical pharmacists to provide appropriate antibiotic selections, ensuring treatment efficacy while minimizing drug side effects and reducing the risk of antibiotic resistance.
To arrange an appointment, please call HOTLINE or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.