Necrotizing cholecystitis is one of the dangerous complications of acute cholecystitis. This condition requires immediate emergency treatment and surgery to address the infection before it threatens the patient's life.
1. Overview of Necrotizing Cholecystitis
1.1. What is Cholecystitis?
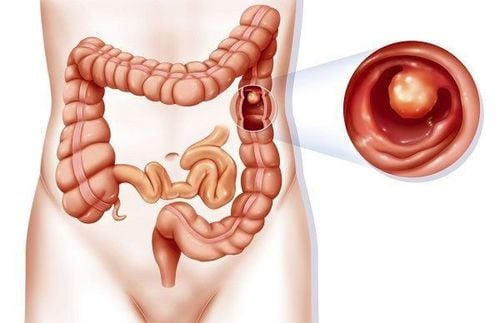
The gallbladder is a small pouch located under the right lobe of the liver, playing a significant role in aiding the digestive process. Cholecystitis refers to inflammation and infection of the gallbladder, primarily caused by gallstones, worms migrating into the bile ducts, tumors, diabetes, infection by E. coli bacteria, or abdominal trauma near the gallbladder region.
There are two types of cholecystitis based on its nature
- Acute cholecystitis: This occurs suddenly, with initial symptoms including sharp pain in the right upper abdomen, often caused by infection of the gallbladder and bile duct obstruction. The pain lasts longer and intensifies with coughing or sneezing.
- Accompanying symptoms include nausea, vomiting, loss of appetite, fever, and jaundice.
- Chronic cholecystitis: This refers to repeated inflammation of the gallbladder. If acute cholecystitis resolves, it may either progress to chronic cholecystitis or not. Symptoms are generally milder but persist over time. Symptoms include bloating, dull abdominal pain, chest tightness, fatigue, and loss of appetite.
1.2. What is Necrotizing Cholecystitis?
Necrotizing cholecystitis is the condition in which part of the gallbladder tissue dies due to infection or inflammation (often related to gallstones or worms in the bile ducts). Necrotizing cholecystitis is one of the dangerous complications of acute cholecystitis. Specifically, when the gallbladder becomes inflamed, the pressure inside increases, compressing the blood vessels that supply blood to the gallbladder. As a result, blood flow to the gallbladder and surrounding tissues is obstructed, leading to cell death due to lack of nourishment.
Necrotizing cholecystitis tends to occur more often in men, individuals with cardiovascular diseases, and those with elevated white blood cell counts. Other risk factors include diabetes, high CRP levels, and severe other diseases.
Patients with necrotizing cholecystitis require gallbladder removal surgery to avoid life-threatening complications.

2. Symptoms of Necrotizing Cholecystitis
When the gallbladder shows signs of necrosis, the patient will exhibit the following symptoms:
- Severe pain in the right upper abdomen, which worsens after eating. The pain may spread around the abdomen or even to the shoulder or arm.
- Nausea and vomiting often occur when the liver produces large amounts of bile but the patient's body cannot store and digest it properly. The patient will experience bloating, indigestion, nausea, and continuous vomiting.
- Jaundice occurs when the gallbladder is necrotic and can no longer store bile. This causes bile pigments to enter the bloodstream, which then spreads to the skin and the whites of the eyes, resulting in yellowing of the skin and eyes.
- Diarrhea and vomiting are also signs of necrotizing cholecystitis. The patient usually experiences diarrhea after eating, especially when consuming fatty foods. Diarrhea may last from a few hours to several days.
- High fever or chills is a common symptom of gallbladder necrosis (a full-body infection).
3. Dangers of Necrotizing Cholecystitis
Necrotizing cholecystitis is considered a high-risk condition. If not diagnosed and treated promptly, it can lead to pus-filled inflammation of the gallbladder, causing perforation or rupture. This may form an abscess, resulting in peritonitis, sepsis, multi-organ failure, and may ultimately threaten the patient's life.
According to statistics, the complication rate of necrotizing cholecystitis ranges from 16% to 25%, with a mortality rate of up to 22%. Among these cases, gallbladder perforation accounts for about 10-15% of all cases. The progression of acute cholecystitis is very rapid, with patients potentially experiencing gallbladder perforation within 2-3 days of bile obstruction.
4. Treatment of Necrotizing Cholecystitis
Necrotizing cholecystitis needs to be treated promptly to prevent unpredictable complications. Key guidelines for patients include:
4.1. What to Do When Signs of Gallbladder Necrosis Appear?
If symptoms of acute cholecystitis, such as right upper abdominal pain, chills, high fever, nausea, and vomiting, occur, the patient should immediately visit a healthcare facility for timely examination and diagnosis. If diagnosed as acute cholecystitis, the patient must receive immediate treatment to avoid the risk of necrotizing cholecystitis and gallbladder perforation. If complications arise, the patient will be recommended to undergo gallbladder removal surgery as soon as possible. Surgery should be performed within 72 hours after the administration of antibiotics.

4.2. Gallbladder Removal Surgery
In cases of gallbladder necrosis, the doctor will typically prioritize surgery for the patient. The surgery involves removing the gallbladder along with any dead or diseased tissue. There are two surgical methods:
- Laparoscopic cholecystectomy: This is the most widely used surgical method. The surgeon makes three or four small incisions (about 10mm each) on the patient’s abdominal wall, through which a laparoscope and instruments are inserted to remove the gallbladder. This procedure is relatively gentle, and patients typically feel minimal pain after surgery, with a quick recovery time.
- Open cholecystectomy: This is the traditional surgical method. The surgeon makes a large incision in the abdomen to expose and remove the gallbladder. Patients who undergo open surgery typically need to stay in the hospital for 7-10 days and may take about 6 weeks to fully recover.
If any of the following abnormal signs occur, the patient should immediately seek medical attention:
- Swelling, pus, or discharge from the surgical site.
- Heat and pain at the incision site.
- High fever (38°C or higher).
- Persistent diarrhea.
- Sudden, severe abdominal pain.
5. Post-Surgical Care for Necrotizing Cholecystitis Patients
After gallbladder removal surgery, patients should follow a healthy and scientific diet, including:
- Eat soft, easily digestible foods that are low in salt during the initial recovery phase. As the body adjusts, patients can gradually return to a normal diet.
- A low-fat diet (around 40-50g of fat per day), such as low-fat milk, lean meats, poultry, vegetables, fruits, fish, and low-fat yogurt, to reduce the risk of digestive disorders, bloating, and indigestion.
- Include unsaturated fats such as fish oil and olive oil to help the liver secrete bile in a natural rhythm according to meals, avoiding bile excess or deficiency.
- Avoid foods high in cholesterol, such as fatty meats, egg yolks, organ meats, certain seafood, fast food, and fried foods, to reduce the risk of gallstone recurrence or digestive issues.
Necrotizing cholecystitis is a dangerous complication of acute cholecystitis. Without timely diagnosis and gallbladder removal surgery, patients can face fatal consequences. Therefore, if symptoms suggesting cholecystitis appear, patients should promptly visit a doctor for early diagnosis and intervention to avoid serious complications.
To arrange an appointment, please call HOTLINE or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.