1. Causes of Bladder diverticulum
Bladder diverticula form when the mucosal layers of the bladder herniate through the muscular layer of the bladder. In most cases, the diverticula are located on the posterior wall of the bladder.
Bladder diverticulum can result from congenital or acquired causes:
- Congenital causes often occur during the bladder's development in children. These diverticula are typically located near the ureteral orifice. Excessive compression of the ureter by the diverticulum can affect the ureter, leading to conditions such as vesicoureteral reflux or ureteral dilation.
- Acquired causes are predominantly seen in adults. Initially, the bladder is structurally normal, but obstructed urinary outflow increases bladder pressure over time. This heightened pressure eventually leads to the formation of bladder diverticulum.

2. Local complications of Bladder diverticulum
The wall of a bladder diverticulum comprises only the mucosal and serosal layers, lacking muscular tissue. Additionally, the neck of the diverticulum is typically narrow, causing urine to stagnate within the diverticulum over time. This chronic urine retention can lead to various complications, including:
- Chronic urine retention
- Urinary tract infections
- Bladder stones
- Pelvic pain
- Acute or chronic urinary retention
- Urination disorder
- Bladder tumors
3. Diagnosis of Bladder diverticulum
There are several diagnostic methods available for bladder diverticula, applicable to both men and women.
3.1. Physical Examination
Physical examination is a commonly used method in diagnosing conditions of the urinary system. This involves the physician using observation, palpation, and percussion to identify abnormalities in the patient's urinary system. Based on clinical symptoms, the doctor may also recommend additional tests such as blood tests, urine tests, or cellular biopsies to achieve the most accurate diagnosis.
For female patients with bladder diverticulum, the physician may examine the vaginal wall to detect masses underneath. Additionally, this method can be used to drain pus or stagnant urine from the diverticulum, aiding in diagnosis and initial management.

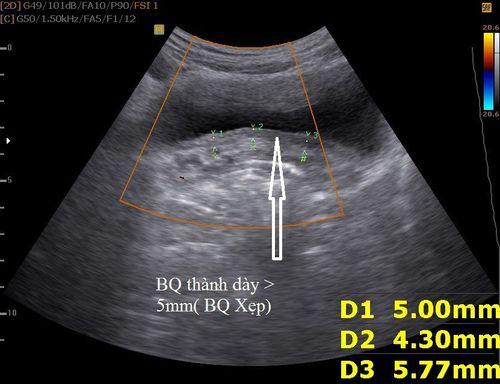
3.2. Ultrasound
Ultrasound is a widely used imaging technique for diagnosis. Through pelvic ultrasound, the doctor can easily visualize the presence of a bladder diverticulum if it exists.
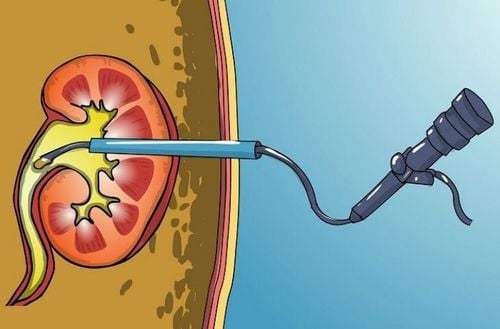
3.3. Cystoscopy
Cystoscopy is a commonly used method for both diagnosing and treating urinary tract conditions. In this procedure, a cystoscope (a thin, flexible tube with a camera) is inserted into the bladder through the urethra.
The physician can easily observe the bladder wall directly or on a screen to check for the presence of a bladder diverticulum. Additionally, with this technique, the doctor can take a small tissue sample from the bladder mucosa for biopsy, aiding in the diagnosis of urinary tract diseases.
3.4. MRI, X-ray of the bladder, and voiding cystourethrography
Magnetic Resonance Imaging (MRI) is considered an excellent diagnostic tool for detecting bladder diverticula in both men and women. Additionally, X-ray imaging of the bladder is also a reliable method for diagnosing bladder diverticulum.
3.5. Double balloon urethral pressure profile
This method is somewhat similar to the X-ray imaging of the bladder and urinary tract described earlier. However, it uses a special catheter to diagnose urethral diverticulum, offering an accuracy rate of 90%.
Since this is an invasive diagnostic procedure, it can cause significant discomfort to the patient and usually requires anesthesia. As a result, it is not commonly used and is not considered a first-line diagnostic tool.

4. Treatment of Bladder diverticulum
There are numerous treatment options available for bladder diverticula, and patients can choose based on their specific condition.
- Complete removal of the bladder diverticulum.
- Incising the neck of the diverticulum and removing all the contents inside.
- Using the Spence technique, creating a pathway from the diverticulum to the vagina.
Bladder diverticulum surgery can be performed through open surgery, removing the diverticulum entirely from outside or inside the bladder. The doctor may also combine it with opening the bladder and closing the diverticulum neck after removal.
If the diverticulum is congenital and affects the ureter, surgery to reimplant the ureter is necessary. For smaller diverticula, the doctor may opt for endoscopic surgery through the urethra and make an incision at the neck of the diverticulum.
For secondary diverticulum, the cause of the obstruction in the lower urinary tract must be removed, and bladder pressure should be reduced.
Depending on the patient's condition, the doctor will provide recommendations for the surgical approach. After surgery, the patient will be prescribed antibiotics for at least 24 hours and may have a catheter inserted to maintain the shape of the urethra for a few weeks. The catheter will be removed based on the recovery progress.
Any surgery can come with complications or side effects. For bladder diverticulum surgery, potential side effects include significant bleeding, recurrence of the diverticulum, infection, urethral scarring, and urinary fistula. The patient should discuss the procedure thoroughly with the doctor before making a decision.
To arrange an appointment, please call HOTLINE or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.