Cerebral infarction and cerebral hemorrhage are two commonly encountered clinical scenarios in the context of cerebrovascular disease, also known as a stroke. Although they have almost similar symptoms, cerebral infarction and cerebral hemorrhage are entirely different phenomena. It is essential to have specific ways to differentiate between cerebral infarction and cerebral hemorrhage in clinical practice to ensure effective diagnosis and treatment for each patient.
1. Cerebral Infarction
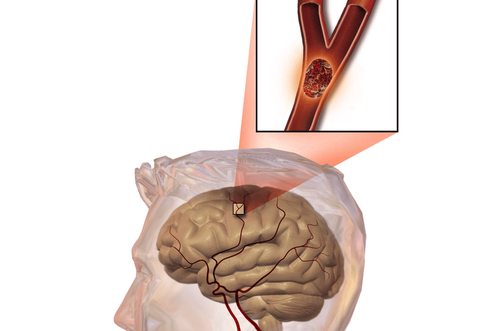
Cerebral infarction, also referred to as focal cerebral ischemia, is characterized by a sudden reduction in blood flow to the brain, leading to partial or complete blockage of the cerebral arteries. Cerebral infarction accounts for the majority of stroke cases, approximately 80%.
If cerebral infarction occurs over a prolonged period, it can result in ischemia, causing brain tissue to lack oxygen and, ultimately, leading to tissue necrosis. This lack of oxygen, or cerebral ischemia, results in severe brain damage, leading to serious complications such as hemiplegia, coma, or disturbances in various body functions, including vision and speech.
The causes of cerebral infarction have been extensively researched and may be due to underlying conditions such as cardiovascular diseases, diabetes, hypertension, atherosclerosis, and lipid metabolism disorders. Although it makes up a large percentage of stroke cases, cerebral infarction can be treated effectively, with fewer dangerous sequelae and lower mortality rates compared to cerebral hemorrhage.

2. Cerebral Hemorrhage
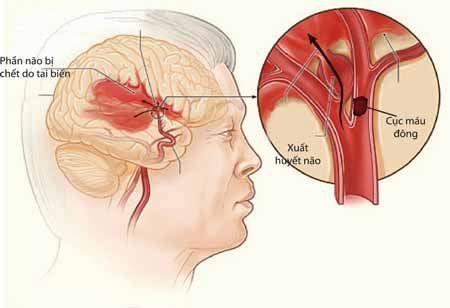
Cerebral hemorrhage, also known as intracerebral hemorrhage, is another case of cerebrovascular accident caused by the sudden rupture of arterial blood vessels into the brain parenchyma, resulting in acute brain injury. While the incidence of cerebral hemorrhage is much lower than cerebral infarction, accounting for only about 20%, it carries a higher risk and severity of complications and mortality.
The mechanism behind cerebral hemorrhage can be explained by the occurrence of trauma, which provocatively increases blood within the brain tissue, leading to cerebral edema. Cerebral hemorrhage results in blood clot formation, increasing pressure on the brain tissue, and ultimately reducing blood flow to the brain, leading to cell death.
Cerebral hemorrhage can occur in various locations, such as within the brain, between brain layers, or even in the membranes surrounding the brain, as well as in the space between the skull and the brain's cortex. The causes of cerebral hemorrhage often include traumatic brain injury, hypertension, obesity, lack of physical activity, and vascular malformations such as brain aneurysms or tumors.
Some cases of cerebral hemorrhage can also occur in younger individuals, potentially due to work or life-related stress. Therefore, if symptoms such as persistent headaches occur, patients should not be complacent but should seek reputable medical facilities for examination and neuroimaging to detect and treat conditions early, preventing unwanted complications.
3. Differentiating Cerebral Infarction and Cerebral Hemorrhage
To accurately differentiate between cerebral infarction and cerebral hemorrhage, it is essential to rely on clinical manifestations of the patient, results from necessary examinations, and the patient's medical history for definitive diagnosis:
- Clinically:
Cerebral infarction in different locations may present various symptoms. For instance, if the middle cerebral artery is affected, the patient might experience hemiplegia. Changes in personality, incontinence, or more pronounced weakness in the lower half of the body can occur due to hypoperfusion of the anterior cerebral artery. Patients with posterior cerebral artery damage may experience visual dysfunction leading to blindness.
In the case of cerebral hemorrhage, patients often present with severe headaches, nausea, vomiting, and possibly altered consciousness. Notably, the symptoms of cerebral hemorrhage tend to appear suddenly and progress rapidly. In more advanced stages, fever and signs of meningeal irritation, such as nuchal rigidity or Kernig's sign, can be observed, differentiating it from cerebral infarction.
- Paraclinically:
Patients with stroke need to undergo some necessary clinical tests for diagnosis, such as lumbar puncture and computed tomography (CT) scan of the brain. Results indicate that in the case of cerebral infarction, the cerebrospinal fluid (CSF) will be clear, while in the case of hemorrhagic stroke, the CSF will be yellow.
The CT scan of the brain will show a decrease in density in the affected brain region in cerebral infarction, while in hemorrhagic stroke, there might be an increase in density, along with edema surrounding the area of damage, and there may be blood in the ventricles.

- Underlying Conditions of the Patient
The underlying conditions of patients with cerebrovascular accidents also play an important role in differentiating between cerebral infarction and hemorrhagic stroke. Cerebral infarction is often caused by arterial embolism, frequently occurring in patients with atherosclerosis or an associated arterial infection, or it may be due to conditions such as vasospasm leading to occlusion.
Additionally, there are certain conditions that are risk factors for cerebral infarction, such as congenital heart disease, atrial fibrillation, mitral valve stenosis, rheumatic heart disease, endocarditis, and myocardial infarction. In contrast, hemorrhagic stroke is frequently caused by traumatic brain injury, which may stem from abnormalities in the shape and structure of the cerebral blood vessels, or it could be related to high blood pressure, coagulopathy, or a history of anticoagulant medication use.
4. Conclusion
Clinically differentiating between cerebral infarction and hemorrhagic stroke is extremely challenging, requiring doctors to have expertise and years of experience in this field. Furthermore, the support of clinical tests is essential to reinforce the diagnosis. Patients showing any signs suggesting a cerebral infarction or hemorrhagic stroke should be attentive and seek medical attention as soon as possible to detect stroke risks early.
Currently, magnetic resonance imaging (MRI/MRA) is considered the “gold standard” for stroke screening. MRI is used to examine the condition of most organs in the body, with particular value in capturing detailed images of the brain or spinal nerves. Due to its high resolution and contrast, MRI images allow for the detection of abnormalities hidden beneath the layers of bone that other imaging methods may struggle to reveal. MRI can provide more accurate results compared to X-ray-based techniques (except for digital subtraction angiography, DSA, for vascular assessment) in diagnosing brain diseases, cardiovascular conditions, strokes, etc. Moreover, the MRI process does not produce side effects as seen in X-rays or CT scans.
To arrange an appointment, please call HOTLINE or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.