The patient had had skin ulcers for three years, underwent multiple unsuccessful treatments, even had encountered fraudulent doctors online. However, when he arrived at Vinmec Hospital, the patient was diagnosed with Livedoid Vasculopathy, demonstrating the complexities and challenges in diagnosing this disease.
The 22-year-old male had gone through a lengthy and failed process of determining the etiology and treatment of recurrent skin ulcers in his lower leg.
This condition causes not only a great deal of pain and difficulties, but also reduces his quality of life. The patient had been examined and treated at several large hospitals in Ho Chi Minh City, but the disease had not been identified and treatments were ineffective.That might be because Livedoid Vasculopathy is rare and hard to diagnose, and its symptoms can overlap with those of other disease .

He was desperate and looked for help online, where he found fraudulent doctors. The patient was treated by a fraudulent doctor online; not only did his condition not improve, but the medication caused several side effects. This had negative impacts on his health and finances, as well as losing patient confidence in the patient's treatment plan. This is a cautionary case about being cautious while searching for medical information online; patients should seek advice from medical specialists and respectable medical facilities.

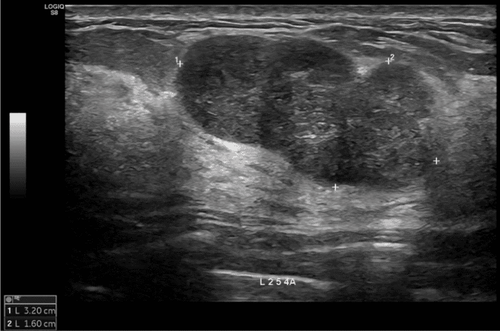
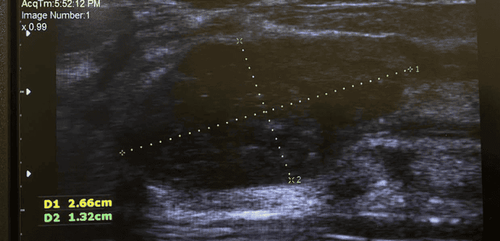
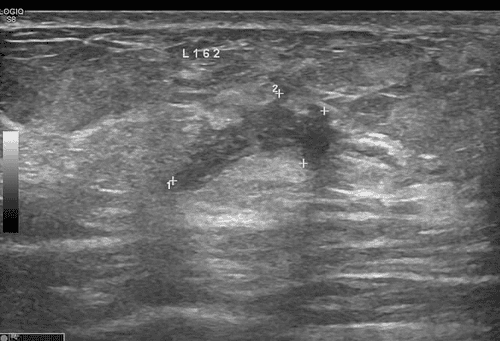
When the patient arrived at Vinmec Central Park Hospital, Dermatodermatologist Quang Lam made a thorough diagnosis. This technique entailed gathering a full medical history, doing a thorough clinical examination, and utilizing appropriate paraclinical diagnostic methods to determine the etiology.
After that, the patient was diagnosed with Livedoid vasculopathy. This is a critical phase that lays the groundwork for establishing a treatment plan.

With understanding and experience in Livedoid Valivedoidhy, Dermatologist Nguyen Quang Lam collaborated with Cardiologist Vu Thi Tuyet Mai to develop a personalized treatment plan based on the patient's unique condition. Anti-inflammatory medications, anticoagulants, topical skin care measures, and supportive therapy are all options for treatment. Patients at Vinmec Central Park Hospital are closely monitored and supervised by interdisciplinary experts during their therapy. This helps to ensure the efficiency of treatment while also monitoring the disease's progression. The patient's condition improved dramatically after only 9 days of treatment.

The case demonstrates the importance of making an accurate diagnosis and selecting the appropriate treatment for patients with rare diseases. It also emphasizes the role of multidisciplinary specialists and specialized medical facilities in ensuring the best diagnosis and treatment for complex diseases such as Livedoid vasculopathy

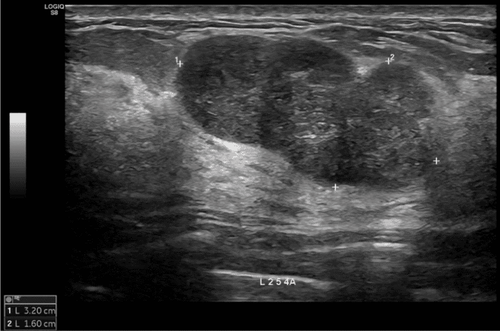
Livedoid vasculopathy is an uncommon skin condition that affects 1/100,000 persons. Livedoid vasculopathy, also known as livedoid vasculitis, is defined by recurrent, painful, poorly healing ulcers in the lower extremities, as well as chronic spider web-like skin lesions (usually dark purple). After healing, the ulcers leave a whitish, pale, sclerotic atrophic scar with varicose veins. The condition is persistent, with repeated acute episodes.
Livedoid vasculopathy is more frequent in women, particularly in their youth and middle years. The exact pathophysiology of Livedoid vasculopathy is unknown, however it is believed to relate to the changing in local or systemic coagulation regulation, as well as localized thrombosis in superficial blood arteries. It is typically treated with antiplatelet, anticoagulant, and fibrinolytic medications. Danazol, stanozolol, PUVA treatment, prostanoids (e.g., alprostadil, PGE-1], and IVIg have all been demonstrated to be successful in some patients.
References:
- Kang S, Amagai M, Bruckner A.L., Enk A.H., Margolis D.J., McMichael A.J., Orringer J.S.(Eds.), (2019). Cutaneous Necrotizing Venulitis. Fitzpatrick's Dermatology, 9e. McGraw Hill.
- Bolognia J.L., Schaffer J.V., Cerroni L(Eds.), (2018). Cutaneous Manifestations of Microvascular Occlusion Syndromes. Dermatology, 4e. ELSEVIER
To arrange an appointment, please call HOTLINE or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.