The article is professionally consulted with Specialist Level I, MD. Trần Minh Tuấn, an ENT specialist and head and neck surgeon in the General Surgery Department at Vinmec Nha Trang International General Hospital.
Peritonsillar abscess and peritonsillar cellulitis are among the most common acute throat infections in teenagers and adults. The symptoms of a peritonsillar abscess include severe sore throat, "hot potato" voice, trismus, and uvular deviation. If not treated promptly, a peritonsillar abscess can lead to dangerous complications.
1. What is a peritonsillar abscess?
A peritonsillar abscess is often a complication of tonsillitis or streptococcal pharyngitis. It is a bacterial infection characterized by a pus-filled pocket near one of the tonsils.
Peritonsillar abscesses usually occur in children, teenagers, and young adults. However, this condition is quite rare because patients are often effectively treated for tonsillitis with antibiotics, preventing the abscess from developing.
2. Symptoms of a peritonsillar abscess
A peritonsillar abscess is a complication of tonsillitis or streptococcal pharyngitis, so the symptoms are similar to those of these conditions. The symptoms of a peritonsillar abscess include:
- Infection occurs in one or both tonsils.
- Fever, with or without chills.
- Difficulty opening the mouth wide.
- Difficulty chewing and swallowing food.
- Difficulty swallowing saliva.
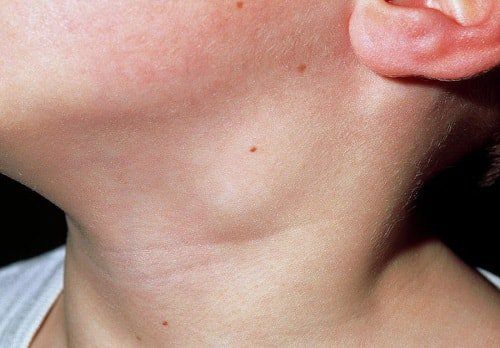
- Swelling in the face or neck.
- Headache.
- Muffled voice.
- Sore throat, usually more severe on one side.
- Swelling in the lymph nodes of the neck or jaw, often painful to touch.
- Ear pain on the same side as the sore throat.
- Bad breath.
Additionally, peritonsillar abscess can cause serious complications, such as:
- Lung infection.
- Airway obstruction.
- Infection spreading to the throat, mouth, neck, or chest.
- Abscess rupture.
If not treated promptly, a peritonsillar abscess can lead to widespread infection throughout the body, possibly even blocking the airways.
3. When to have a medical check-up for a peritonsillar abscess?
If you have a sore throat accompanied by fever or other symptoms, promptly see a doctor for an accurate diagnosis.
Additionally, if you experience symptoms such as a sore throat combined with difficulty swallowing, breathing, speaking, or signs of airway obstruction, you should immediately go to the hospital to avoid life-threatening complications.
4. Causes of peritonsillar abscess
As mentioned above, a peritonsillar abscess is a complication of tonsillitis. It occurs when the infection spreads to the areas surrounding the tonsils and forms an abscess.
Infectious mononucleosis and dental or gum infections can also cause a peritonsillar abscess. In some rare cases, a peritonsillar abscess may not be caused by an infection but by inflammation of the salivary glands.
5. What methods help diagnose a peritonsillar abscess?
Firstly, to diagnose a peritonsillar abscess, a doctor will examine your throat and mouth. Then, the doctor may request a blood test or take a throat fluid sample to confirm the diagnosis. Signs that help diagnose a peritonsillar abscess include:
- Swelling on one side of the throat.
- Swelling on the roof of the mouth.
- Redness and swelling in the throat.
- Enlarged lymph nodes on one side of the neck.
Additionally, the doctor may suggest a CT scan or MRI to get a clearer view of the abscess. The doctor may also use a needle to take a sample of the abscess fluid to identify if there is an infection.
6. Treatment methods for peritonsillar abscess
Generally, doctors will prescribe antibiotics to treat a peritonsillar abscess. Additionally, draining the pus from the abscess can help speed up the healing process. Depending on the stage and symptoms, the doctor will determine the appropriate treatment:
- The peritonsillar cellulitis stage is an intermediate phase between acute tonsillitis and a peritonsillar abscess. In this stage, treatment involves using antibiotics combined with anti-inflammatory, antipyretic, and pain-relieving medications as prescribed.
- When there is pus in the peritonsillar abscess, the treatment involves incising and draining the abscess, keeping the incision open for about 3 days. This is combined with intravenous or injectable antibiotics that target both aerobic and anaerobic bacteria, along with anti-inflammatory, pain-relieving, and fever-reducing medications.
If you can't eat or drink, the doctor may administer intravenous fluids. If your throat is too painful, the doctor may give you pain relief medication. If the abscess recurs, the doctor may recommend a tonsillectomy to avoid more serious complications.

7. How dangerous is a peritonsillar abscess?
A peritonsillar abscess usually resolves without complications if treated properly. However, if left untreated or treated improperly, it can lead to serious complications such as:
- Airway obstruction.
- Dehydration.
- Infections in the jaw, neck, or chest.
- Sepsis.
- Pneumonia.
- Meningitis.
- Endocarditis.
8. Prevention of peritonsillar abscess
The simplest and most effective method to prevent a peritonsillar abscess is to reduce the risk of tonsillitis and pharyngitis by: not smoking, maintaining good oral hygiene, and properly treating oral infections.
Stay updated with other useful information by regularly visiting the website: Vinmec.com.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
To arrange an appointment, please call HOTLINE or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.








