Cervical tuberculous lymphadenitis is a common disease of extrapulmonary tuberculosis. Relapse of tuberculous lymphadenitis is common in HIV/AIDS patients. So are tuberculous lymphadenopathy in general and in specific cervical tuberculous lymphadenitis dangerous?
1. What is tuberculous lymphadenopathy?
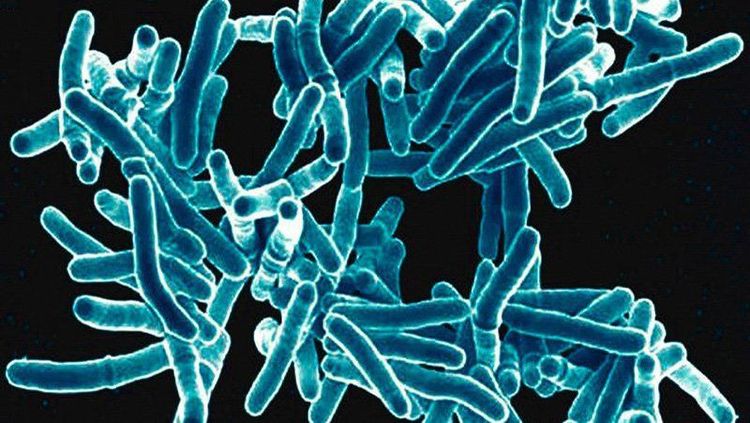
Tuberculous lymphadenopathy is a form of tuberculosis infection occurring outside the lungs, commonly found in children, adults, both men and women. Tuberculous lymphadenopathy is divided into 2 types, depending on the location of the tuberculosis:
- Peripheral tuberculous lymphadenopathy: Neck, armpit, groin.
- Visceral tuberculous lymphadenopathy: Mediastinal, mesentery.
However, peripheral tuberculous lymphadenopathy is more common than visceral tuberculous lymphadenopathy, especially cervical tuberculous lymphadenitis due to mycobacterium tuberculosis entering the damaged nose, mouth, throat and localizing there, causing lymphadenopathy. Therefore, this article focuses on sharing about peripheral tuberculous lymphadenopathy.
2. Symptoms of cervical tuberculous lymphadenitis
Peripheral tuberculous lymphadenopathy may cause systemic symptoms or not. Most patients with tuberculous lymphadenopathy have the following symptoms:
- Mild fever, especially in the afternoon
- Fatigue, loss of appetite, weight loss
- Other organs are affected by tuberculosis including the meninges, lungs,...
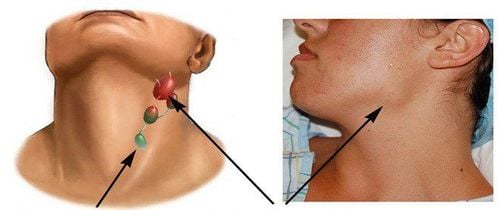
Peripheral tuberculous lymphadenopathy most commonly occurs in the neck, with the common lymph nodes located along the sternocleidomastoid, supraclavicular and submandibular muscles. Cervical tuberculous lymphadenitis is more common on the right side than on the left, mainly on one side, rarely on both sides of the neck.
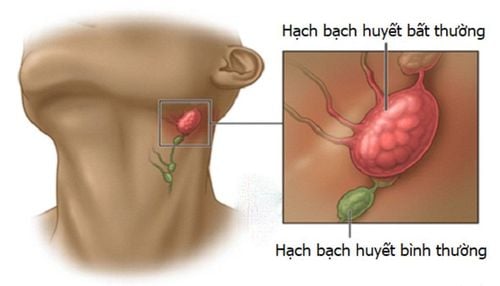
To distinguish it from normal lymph nodes, we can rely on the following characteristics of the size and feature of the lymph nodes:
- The size of the tuberculous lymph nodes is not large (about a few centimeters in diameter), consisting of a chain of lymph nodes
- The lymph nodes can be mobile, soft and tense
- The lymph nodes may or may not be painful
- Depending on the skin area, the lymph nodes may be normal or red and swollen
3. How does cervical tuberculous lymphadenitis progress?
Cervical tuberculous lymphadenitis in particular and tuberculosis in general can progress through the following 3 stages:
- Stage 1 - Swollen lymph nodes: From the outside, you can see a mass of lymph nodes tends to swell because it consists of many lymph nodes of different sizes. The lymph nodes have not yet stuck together or attached to the skin, so when you touch them, the lymph nodes can move.
- Stage 2 - Lymphadenitis: The lymph nodes begin to connect together to form a patch, or they can also stick to the skin and surrounding tissues. At that time, the lymph nodes are more difficult to move.
- Stage 3 - Matting: Tuberculous lymphadenitis in the neck moves to the matting stage, the lymph nodes become softer, the skin area with the lymph nodes is swollen and red, but does not cause pain or heat. After that, the lymph nodes become purulent and rupture. When they rupture, there are purple fistulas on the lymph nodes that take a long time to heal. When the fistulas heal, they cause wrinkled scars that protrude outward, are white in color, or fibrous ligaments can be seen on the scars.
Monitoring and recognition of tuberculosis progression is very important, suggesting and supporting the diagnosis of lymphadenopathy.
4. Treatment of tuberculous lymphadenopathy
Treatment of tuberculosis in general and in specific cervical tuberculous lymphadenitis mostly is internal medicine with the same protocol and principles as tuberculosis, combining at least 3 anti-tuberculosis drugs. If in the intensive phase, it may be necessary to combine up to 4 anti-tuberculosis drugs and in the continuation phase, combine 2 anti-tuberculosis drugs.
Lymphatic tuberculosis is recurrent, so the treatment duration should be maintained for about 9 - 12 months. In addition, the treatment results of tuberculous lymphadenopathy may not be as fast as other forms of tuberculosis because the drug is difficult to penetrate into the tuberculous lymph node lesions.
Tuberculous lymphadenopathy should be treated when the lymph nodes have not ruptured yet. At that time, treatment is done by inserting a needle into the lymph nodes to aspirate the pus and inject drugs. When the lymph nodes rupture, the pus needs to be squeezed out of the lymph nodes every day, then applied medicated gauze.
Rarely treat tuberculous lymphadenopathy in general and cervical tuberculous lymphadenitis in particular by surgery, except in the following cases:
- The lymph nodes are enlarged, red and in the stage of matting, suppuration: Purulent drainage, incision and scraping off the tissue inside the lymph nodes. Combine local medication until the wound dries and heals. This treatment prevents ugly scarring..
- The lymph nodes have purulent discharge but have not been completely squeezed out: Incise and widen the fistula to scrape out all the purulent, then local treatment as above with anti-tuberculosis drugs combined as the treatment of tuberculosis.
- The lymph nodes are enlarged and compress other tissues (blood vessels, nerves): When the lymph nodes are relapse, even swollen and compressed, surgery is needed to remove the lymph nodes, however, when operating the surgery, it’s a necessary precaution that the surrounding blood vessels and nerves are not damaged.
Note, treat tuberculous lymphadenopathy with corticosteroids in cases of multiple tuberculous lymph nodes to reduce inflammation, minimize the size of tuberculous lymph nodes, limit the possibility of discharge pus, reduce abscesses, thereby avoiding surgical treatment.

5. Is tuberculous lymphadenopathy dangerous?
With the characteristics of symptoms, disease progression as well as treatment methods shared above, tuberculous lymphadenopathy is not really dangerous because compared to other forms of tuberculosis, treatment of tuberculous lymphadenopathy in general and cervical tuberculous lymphadenitis is partly simpler.
Children with tuberculous lymphadenopathy when treated with systemic treatment combined with hygiene will recover. However, it should be noted that in the treatment of tuberculous lymphadenopathy in children, the lymph nodes should not be removed too early because at this time the lymph nodes play a role in protecting the body against the invasion of mycobacterium tuberculosis bacilli.
Lymphatic tuberculosis is not contagious like pulmonary tuberculosis. Tuberculous lymphadenopathy can be prevented by keeping the body from being damaged in the mouth and throat area and focusing on improving resistance every day to avoid prolonged lymphadenitis that creates favorable circumstances for bacterium tuberculosis bacilli to invade and cause lymphadenopathy.
Cervical tuberculous lymphadenitis in particular and tuberculosis lymph nodes in general are not dangerous because compared to other forms of tuberculosis, the treatment method is simpler and the disease can be cured when combined with systemic treatment, enhancing immune system and physical health, and simultaneously living and resting properly.
To arrange an appointment, please call HOTLINE or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.
To arrange an appointment, please call HOTLINE or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.