Vaginal yeast infection (also called vaginal candidiasis) is relatively easy to treat but challenging to prevent from relapsing due to the resilience and persistence of the fungal spores. Without proper preventive measures, the infection can frequently relapse.
1. What is Vaginal Candidiasis?
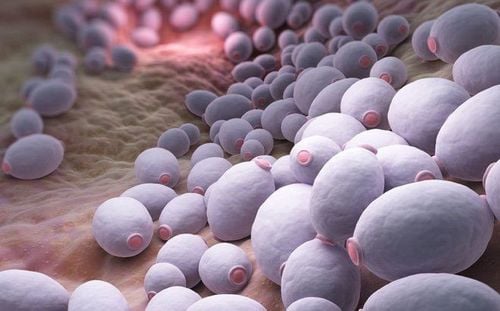
Vaginal candidiasis is a common gynecological condition caused by the yeast Candida albicans. Under normal circumstances, Candida exists in its spore form in the vaginal canal without causing infection. However, certain conditions—such as warm, humid weather or disruptions to the vaginal microbiota—can trigger fungal overgrowth, leading to infection.
Candida is a yeast-like fungus with an oval or round shape, measuring approximately 2–5 μm. It is a commensal organism in the human and animal gastrointestinal tract and vagina. In healthy individuals, Candida is found in approximately 30% of oral cavities, 17% of bronchial passages, 38% of intestines, and 39% of vaginal environments. While Candida can cause infections in various parts of the body, it predominantly affects the skin and mucous membranes, with the vaginal and vulvar mucosa being particularly susceptible in developing a fungal infection from overgrowth.
Vaginal candidiasis is one of the most prevalent gynecological infections. The condition is often linked to prolonged and broad-spectrum use of antibiotics or antifungals, which disrupts the natural vaginal flora. Additionally, pregnancy (especially in the third trimester) and diabetes mellitus can lower vaginal pH, creating a favorable environment conducive for fungal overgrowth.
Women with frequent sexual activity or those using hormonal contraceptives also face an increased risk of developing vulvovaginal candidiasis.
Patients suffering from vaginal candidiasis may exhibit symptoms of: Itching in the vulvar region, burning sensation in the vagina, and painful intercourse. Gynecological inspections may show evidence of inflammation of the vaginal and vulvar mucosa; thick, white, curd-like vaginal discharge. Other lesions may extend to the perineal and inguinal areas.
2. Why Does Vaginal Candidiasis Frequently Relapse?
Successful treatment of vaginal candidiasis requires addressing both the affected woman and her sexual partner. Many women experience recurrent infections due to their partners not receiving simultaneous treatment. Additionally, oversights on personal hygiene practices, such as failing to wash undergarments separately with soap and not drying them in direct sunlight, can contribute to re-infection.
Another significant factor in recurrence is non-compliance with medical treatment. Some patients fail to follow up with post-treatment examinations after their initial drug regimen has been completed, potentially leading to inadequate drug therapy and incomplete fungal decolonisation.
Furthermore, many women willingly purchase over-the-counter antifungal when experiencing itching or abnormal discharge without professional consultation, increasing the risk of antifungal resistance and recurrence.

3. Preventive Measures for Vaginal Candidiasis
Vaginal candidiasis can cause significant itching, burning sensation, discomfort during sexual intercourse, and disrupt quality of life. Since the condition has a high recurrence rate due to fluctuations in vaginal pH, women should adhere to the following preventive measures:
- Schedule regular gynecological check-ups every six months to monitor reproductive health. Seek medical attention if experiencing symptoms such as abnormal vaginal discharge, burning sensation, pruritus, dysuria, or lower abdominal pain.
- Maintain proper hygiene by keeping the vaginal area clean and dry to inhibit fungal growth.
- Avoid excessive vaginal douching, as it can damage the mucosa, disrupt the vaginal microbiota and pH. Avoid over-reliance on feminine hygiene products with high moisturizing content or strong antibacterial agents.
- Wear breathable cotton underwear and avoid tight-fitting, non-absorbent garments that create a moist environment conducive to fungal proliferation.
- Use high-quality sanitary pads and change them frequently during menstruation to prevent bacterial and fungal infections.
- Ensure proper drying and hygiene of clothes and underwears by washing them separately and drying in direct sunlight.
- Seek medical consultation and adhere to prescribed treatments if diagnosed with a fungal infection.
- Abstain from sexual intercourse during an active infection to prevent transmission and worsening symptoms.
- Both partners should undergo antifungal treatment if the female partner is diagnosed with vaginal candidiasis. The fungal spores may survive and remain on the male’s penis after each intercourse and may reintroduce the yeast infection to his partner in subsequent intercourses.

Vaginal candidiasis is highly recurrent due to the persistence of fungal spores on clothing and in the environment. Therefore, women should seek medical evaluation if they notice any abnormal vaginal symptoms. Early detection and appropriate treatment can prevent complications and reduce recurrence rates.
To support early diagnosis and effective treatment of vaginal candidiasis and other gynecological conditions, Vinmec International General Hospital offers a Comprehensive Gynecological Screening Package. This package enables early detection of infections, allowing for timely and cost-effective treatment. It also includes screening for gynecological cancers, such as cervical cancer, even before symptoms appear.
This screening package is available to all women, regardless of age, and is recommended for those experiencing:
- Unexplained vaginal bleeding
- Menstrual irregularities: prolonged menstruation, irregular menstruation
- Abnormal vaginal discharge (foul odor, unusual color)
- Vulvar itching or pain
- Poor personal hygiene habits, unsafe sexual practices, or a history of surgical abortions
- Any patients with symptoms of abnormal vaginal discharge, vulvar pain and abnormal vaginal bleeding.
To arrange an appointment, please call HOTLINE or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.