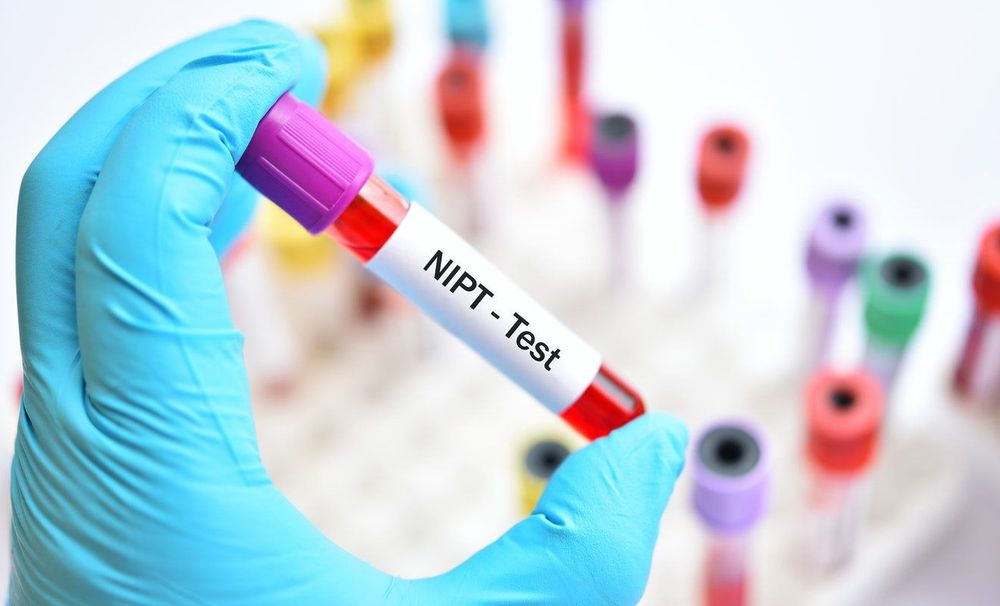
NIPT is a non-evasive screening test that is increasingly used and has a very high value for prenatal screening. However, when undergoing and interpreting the test results, pregnant women need to understand certain information about the test's value. It is especially important to understand that any test has a certain rate of false-positive and false-negative results. For NIPT, the positive predictive value for common trisomies is around 90%. This can be simply understood as approximately 10% of women with abnormal test results actually have a normal fetus. So, what are the causes of false-positive and false-negative results in NIPT?
1. Causes of false-positive results in NIPT
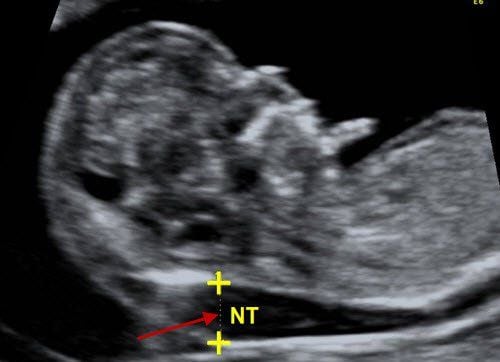
- Placental mosaicism: Since the primary source of free fetal DNA in the maternal circulation is from placental cells (syncytiotrophoblasts), NIPT essentially provides results related to the placenta, which may differ from the fetal tissue. Mosaicism occurs in 1 to 2 percent of pregnancies and is more likely to be associated with Turner syndrome (XO) and trisomy 13 than trisomy 21 or 18.
- In the case of twin pregnancies with one fetal demise or vanishing twin syndrome: This occurs because the placenta of the deceased fetus may still be present at the time of the test, continuing to release DNA into the maternal circulation weeks after fetal death.
- Maternal mosaicism: Most cfDNA testing methods assume that the mother has a normal karyotype, but this is not always true. For example, with increasing age, the number of cells with missing X chromosomes in a woman’s body increases, which can lead to false-positive cfDNA results. Additionally, although rare, some women may have sex chromosome abnormalities (e.g., 47, XXX) but exhibit a normal phenotype. Maternal mosaicism can be diagnosed through karyotyping of peripheral blood lymphocytes, and because of that, it is relatively easy to identify the cause of a false-positive result.
- Maternal cancer – Tumor-derived free DNA (ctDNA) can be released into the maternal circulation at detectable levels in women with malignancies. In a pregnant woman with a tumor, both fetal free DNA and ctDNA from the tumor contribute to the total cfDNA, which can lead to false-positive results. In a study of 450,000 pregnancies tested, 55 cases of potential maternal cancer were identified. Among these, 40 cases were confirmed as maternal tumors, with 20 cases being benign uterine fibroids, 18 cases being malignant tumors, and 2 cases unclassified. However, not all cfDNA testing laboratories are able to detect patterns suggesting maternal cancer. Some laboratories providing cfDNA tests that assess the likelihood of cancer in the mother may refer clients for further oncological examination when unusual results are found. The most common malignancies in women of reproductive age include breast cancer, cervical cancer, ovarian cancer, colorectal cancer, leukemia, Hodgkin's and non-Hodgkin lymphoma, thyroid cancer, and melanoma. However, NIPT should not be considered a screening test for maternal malignancies, as there is limited data on this correlation.
- Maternal genetic material variants: The cfDNA analysis method assumes that all women have the same proportion of genetic material on a particular chromosome, but in reality, chromosomes can vary slightly between individuals. In such individuals, cfDNA sequencing method may yield positive results when the maternal duplication size is relatively large and occurs on a chromosome of interest (e.g., chromosome 21).
- False-positive rates may also result from statistical probability, as the threshold for a positive test is usually set at +3 standard deviations. Therefore, 1 or 2 out of 1,000 monosomic fetuses may have a false-positive result, and if 100,000 tests are performed, it is estimated that there will be 100 false-positive NIPT results.
- Technical issues: Like all laboratory tests, rare sample mixing or other technical errors can lead to false-positive (or false-negative) test results.
- Transplant recipients: If the transplanted tissue (bone marrow or organ) is taken from a male donor, cfDNA testing may incorrectly identify a female fetus as male due to the release of male cfDNA from the transplanted organ into the maternal circulation.
- Recent blood transfusion: If the mother has received blood from a male donor less than 4 weeks before the cfDNA blood sample is taken, the test may incorrectly identify the fetus as male.
2. Causes of false-negative results in NIPT
NIPT is a screening test that is increasingly used and has a very high value in prenatal screening. However, when undergoing this test or interpreting its results, pregnant women need to understand some information about the value of NIPT, especially recognizing that any test has a certain rate of false positives and false negatives. For NIPT, there are cases where false negatives may occur (the test result indicates normal, but the fetus actually has a genetic abnormality). According to many studies, the false negative rate of NIPT is approximately 5%. So, what causes such false negative results? Possible reasons include:
- Fetal mosaicism: The primary source of "fetal" cfDNA in the maternal circulation is placental cells (trophoblasts, syncytiotrophoblasts). This DNA may differ from the DNA of fetal tissue. There are cases where a fetus has an aneuploid karyotype, even though the placental karyotype is normal, leading to a test result indicating normality. This is common in trisomy 13 and 18 and rarely occurs in trisomy 21.
Low fetal cfDNA fraction at the threshold: Although there may be a sufficient amount of total cfDNA for the test to identify, the proportion of fetal cfDNA is at the lower limit (typically below 4%), resulting in minimal differences between the reference ratios of a normal individual and the observed and analyzed chromosomal fragment ratios (e.g., fragments of chromosome 21). Without enough DNA fragments, these differences cannot be detected, leading to a false-negative screening result that is reported inaccurately. This phenomenon is commonly observed in cases where the mother is using low molecular weight heparin (LMWH), such as enoxaparin, in obese mothers, or when the test is conducted early before 10 weeks of pregnancy. - Maternal genetic material variations: The cfDNA analysis method assumes that all women have the same proportion of genetic material on a given chromosome. However, in reality, chromosomes vary slightly between individuals. In some cases, theoretically, the maternal loss of genetic material could result in a false-negative outcome. However, this is much rarer than false positives because the fetal aneuploidy and the maternal deletion would need to involve the same chromosome.
- Technical issues: Technical issues in testing techniques can make it more difficult to detect certain aneuploidies. For instance, the low guanine-cytosine (GC) content of chromosome 13 makes polymerase chain reaction (PCR) steps and subsequent sequencing less reliable. This results in a lower detection rate compared to other aneuploidies. Laboratories attempt to correct this through bioinformatics analysis, but these efforts are not always successful. Additionally, sample mix-ups or other laboratory-related issues can sometimes lead to false-negative NIPT results.
Therefore, although NIPT is currently a highly accurate test, it is still considered a screening test rather than a diagnostic one. Pregnant women should still be closely monitored by obstetricians and undergo regular fetal ultrasounds to detect abnormalities early and determine appropriate interventions and treatments.
To arrange an appointment, please call HOTLINE or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.