1. Overview
Cervical spondylosis is the natural aging process of the spine, affecting the cartilage, intervertebral discs, ligaments, and bones in the cervical spine region. This condition often leads to neck pain, especially when moving the neck, causing stiffness and other symptoms.

It is a fairly common chronic condition and may appear in patients as early as 30 years old. In particular, up to 90% of patients over the age of 60 suffer from cervical spondylosis. This condition progresses slowly and can occur in any segment of the spine. However, the C5, C6, and C7 vertebrae are the most commonly affected locations.
2. Is cervical spondylosis dangerous?
Cervical spondylosis is a very common condition. Not only the elderly but also younger individuals, especially office workers, people who move infrequently, or those who often bend their necks, are at risk of developing this condition.
People who frequently perform activities involving the head and neck area are also susceptible to this condition. The disease causes many difficulties in daily activities and work. In addition, the incidence rate between men and women is nearly equal.
3. Causes of cervical spondylosis
Cervical spine degeneration occurs due to one of the following causes:
3.1 Incorrect posture
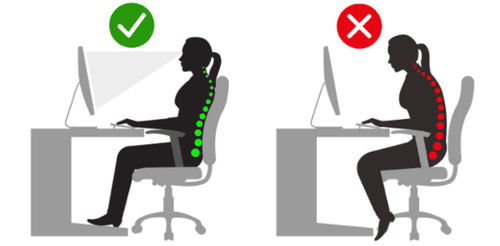
Incorrect posture is one of the main causes leading to cervical spine degeneration. Working for long periods in one position and lack of movement are important factors contributing to this condition.
Jobs that require frequent bending, stretching, carrying heavy loads on the head, or sitting in front of a computer for too long can also lead to cervical spine degeneration, spinal calcification, and bone spurs.
3.2 Nutrition
Cervical spondylosis can also result from an inadequate diet. Causes include poor nutrition and decreased levels of calcium, magnesium, and vitamins in the body.
3.3 Medical conditions
Certain medical conditions can cause cervical spine degeneration, specifically:
- Disc dehydration: The intervertebral discs act as cushions between vertebrae. By the age of 40, most discs begin to dry out and shrink. This causes the vertebrae to rub against each other more and move less smoothly.
- Herniated disc: Tears or cracks appear in the disc, causing herniation. Sometimes this condition can compress and damage the spinal cord and nerves.
- Ligament thickening: Ligaments connect bones together. Over time, ligaments may thicken with age, making the neck less flexible and contributing to cervical spondylosis.
- Bone spurs: Degenerating discs can cause excessive bone growth along the spine, forming bone spurs. These spurs may occasionally compress the spinal cord and nerves.
3.4 Lifestyle
Some daily habits and work-related factors that may cause cervical spine degeneration include:
- Using a computer for long periods with little movement
- Desk height being too high or too low
- Rarely moving the neck or keeping it in one position too long
- Frequently bending or extending the neck
- Sitting too low compared to the desk or having a screen positioned too high or too low
- Excessive use of alcohol and smoking
- Sleeping in only one or two positions without changing sides
- Using inappropriate pillows (too high or too soft)

4. Symptoms of cervical spondylosis
Most cases initially show no specific symptoms. When symptoms appear, the most common include:
- Fatigue and soreness
- Difficulty moving the neck
- Sharp pain even at rest
- Pain during movement
Although patients may not feel abnormalities at first, other symptoms may develop later, such as:
- Pain or stiffness during neck movements, sometimes leading to torticollis
- Pain radiating from the nape to the ears and neck, affecting posture, causing the head and neck to tilt
- Pain radiating to the head, particularly in the occipital or frontal areas
- Pain radiating from the neck to the shoulders and arms, on one or both sides
- Stiff neck in the morning after sleeping in an uncomfortable position or during cold weather
- Numbness or heaviness in the arms and hands, sometimes progressing to paralysis
- Neck stiffness, difficulty walking, or fear of sneezing and coughing due to pain
- Dull aching pain in the nape or back of the head, spreading to one side
- Continuous pain, inability to turn the head without rotating the entire body
Additionally, patients with cervical spondylosis may experience Lhermitte’s sign—a symptom of multiple sclerosic-related cervical spine degeneration, also called the “barber’s chair phenomenon.”
Lhermitte’s sign is a sudden unpleasant sensation like an electric shock running from the neck down the spine, sometimes radiating to the arms, legs, fingers, and toes. This sign becomes stronger when bending forward and may last briefly or for a longer duration.
5. Factors increasing the risk of cervical spondylosis
Some factors that increases the risk of cervical spondylosis incldues
5.1 Age
Older adults are at higher risk. Cervical spondylosis commonly occurs in middle-aged individuals (40–50 years).
At this age, decreased blood flow causes intervertebral disc and vertebral body degeneration.
5.2 Occupation
People who work in positions requiring frequent neck movement or bending, high labor intensity, and long careers are more likely to develop cervical spondylosis.
High-risk groups include:
- Farmers (more prone to cervical and lumbar degeneration)
- Hairdressers
- Dentists
- Construction workers (painters, plasterers)
- Circus performers
- Office workers
Among these, office workers are at the highest risk due to prolonged sitting, limited movement, and insufficient rest.
5.3 Other causes
- Neck injury: Past neck trauma increases risk.
- Genetics: Having family members with cervical spondylosis raises the likelihood of developing the condition.
- Smoking: Smoking increases the risk of neck pain.
6. Prevention of cervical spondylosis
Cervical spine degeneration is closely related to occupational habits. Therefore, prevention during work stages can minimize risk. Specifically:
- Regularly massage and care for the neck area, avoid overwork, and maintain balance between labor and rest.
- Office workers should protect their health through simple exercises and frequent posture changes.
- Avoid sitting at a computer for long periods and maintain a balanced diet. Chair height should be adjusted to desk and body height.
- Use screens of at least 17 inches and maintain a 50–66 cm distance, placing the screen 10–20° below eye level.
- Ensure the screen is not too high or low relative to eye level.
- Keep arms parallel to the desk, back straight, and shoulders level.
- When sleeping, change positions regularly; avoid lying prone or using high pillows.
- Do not twist or press the neck forcefully. Use a moderately thick pillow to avoid excessive bending or extension.
Patients should also note the following:
- Change sitting posture regularly when using computers or watching TV.
- Avoid sudden twisting of the neck.
- Do not carry heavy objects on the head.
- Avoid bending the neck for prolonged periods when reading or watching TV.
- Use seats with head and back support when traveling long distances.
- Massage under medical supervision.
- Perform gentle exercises.
If experiencing pain radiating to the arms or signs of limb weakness, do not attempt self-massage or strong manipulation; seek a neurologist for accurate diagnosis and treatment.
7. Diagnostic methods for cervical spondylosis
Diagnosis includes clinical and paraclinical examinations:
7.1 Clinical examination
A clinical diagnosis can be made when the physician:
- Assess range of neck motion.
- Test muscle strength and reflexes in the arms to determine if nerves or the spinal cord are affected.
7.2 Imaging tests
Imaging studies can provide further evaluation to reach a definitive diagnosis and treatment, they include:
- X-ray: Detects abnormalities such as bone spurs or bridges, indicating degeneration, and helps rule out rare and more serious causes like tumors, infections, or fractures.
- CT scan: Provides more detailed images, especially for small bone lesions.
- MRI: Identifies herniated discs and nerve compression.
7.3 Nerve function tests
Additional tests may determine whether nerve conduction is affected:
- Electromyography (EMG): Measures electrical activity in nerves during muscle contraction and rest.
- Nerve conduction studies: Electrodes placed on the skin deliver small currents to assess signal strength and speed.
8. Treatment of cervical spondylosis
Treatment depends on severity and symptoms. The goal is to relieve pain, maintain daily function, and prevent permanent spinal cord and nerve damage.
8.1 Medical treatment
Medications can be prescribed for treatment. They include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs), choosing the right type of medication is dependent on patient health and comorbidities
- Corticosteroids: Short oral courses or local injections may be used for severe pain.
- Muscle relaxants such as cyclobenzaprine to relieve spasms.
- Anticonvulsants such as gabapentin (Neurontin, Horizant) or pregabalin (Lyrica) to reduce nerve pain.
- Antidepressants: some have been proven to relieve chronic neck pain.
8.2 Physical therapy
Exercises to relax and strengthen neck and shoulder muscles. Techniques include stretching, massage, and iontophoresis for pain reduction.
8.3 Surgery
If conservative treatment fails or neurological symptoms persist, surgery may be necessary to decompress the spinal cord and nerve roots.
Surgical options include:
- Removing a herniated disc or part of a vertebra
- Partial vertebral removal
- Spinal fusion by grafting vertebrae together
With many years of experience in musculoskeletal and orthopedic surgery, Vinmec International General Hospitalhas become one of the leading centers for advanced diagnosis and treatment.
When symptoms of cervical spondylosis is apparent, patients can visit Vinmec for consultation, diagnosis, and treatment to ensure quick recovery. Specialists in Internal Musculoskeletal Medicine and Orthopedic Surgery will collaborate to perform advanced diagnostic methods and prescribe appropriate treatment plans.
To arrange an appointment, please call HOTLINE or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.