The article is professionally consulted by Dr. Pham Thi Yen - Grade I Specialist - Obstetrics and Gynecology Specialist - Department of Obstetrics and Gynecology - Vinmec Hai Phong International General Hospital.
The cervix is the section preceding the entrance to the uterine cavity and is quite susceptible to trauma, particularly during vaginal delivery. Consequently, cervical laceration necessitates immediate intervention following the completion of labor to prevent complications and minimize future sequelae.
1. What is cervical laceration?
The uterus is an organ composed of thick smooth muscle layers, serving as the implantation site for a fertilized egg and the developmental environment until the fetus reaches maturity. The uterus has a truncated cone shape, with a broad upper base and a narrow tip directed downward, consisting of three parts: the body of the uterus, the isthmus, and the cervix.
The normal cervix measures approximately 2 to 3 cm in length and 2 cm in width. In nulliparous women, the cervix and the external os are round and firm in consistency. After one childbirth, the cervix flattens, and the external os becomes slightly enlarged, losing its round shape and becoming softer. With subsequent births, the external os of the cervix will continue to widen laterally.

During labor, as a result of uterine contractions, the cervix transforms from a cylindrical shape into a thin plate. This process, known as cervical effacement, occurs concurrently with cervical dilation, facilitating the formation of the lower uterine segment, which allows for easier expulsion of the fetus. At this point, any excessive stretching of the pelvic floor or procedural interventions during delivery can easily lead to complications, including cervical laceration.
Cervical laceration may exist as an isolated injury or may be accompanied by vaginal and perineal lacerations. Furthermore, the classification of cervical laceration can vary depending on the position of the laceration on the transverse plane through the cervix or its anatomical location relative to the vaginal wall. If the cervical laceration is below or above the attachment to the vaginal wall, the extent of injury is often mild, with minimal bleeding. Conversely, if the laceration occurs directly on the cervix, the injury is usually severe, leading to significant hemorrhage, potentially resulting in hypovolemic shock and life-threatening complications.
2. Causes of cervical laceration
Anatomical abnormalities and incompatibilities in the physiology of labor contribute to the risk of cervical laceration. Notably, an oversized fetal head may compress the cervix, while premature pushing by the mother when the cervix has not fully dilated, prolonged labor, and repeated examinations can weaken the cervix, making it vulnerable to damage, even with relatively modest forces applied.
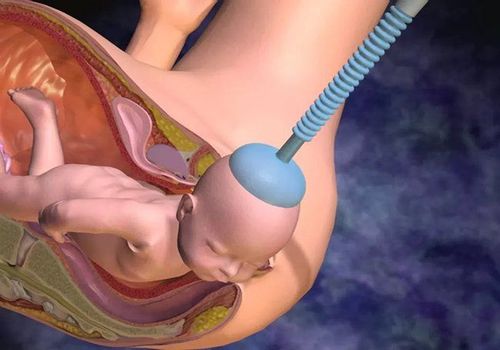
Additionally, the use of instruments to assist labor, such as vacuum extraction or forceps, to expedite fetal delivery can inadvertently result in trauma to the cervix.
Moreover, a vaginal delivery presents a higher risk of cervical laceration if the woman has a history of cervical pathology, such as infections, cervical scarring due to prior injuries, previous lacerations, conization, or multiple electrosurgical interventions on the cervix.
3. How to diagnose cervical laceration?
Following a spontaneous vaginal delivery, the pain caused by uterine contractions and heightened mental focus, combined with the effects of local anesthesia and spinal anesthesia, results in the patient experiencing minimal sensation in the lower extremities. Consequently, cervical laceration is primarily identified through the continuous presence of postpartum hemorrhage. The volume of bleeding may vary depending on the nature of the laceration, its location, depth, and its relationship with surrounding structures. At this stage, it is crucial to differentiate cervical laceration from atony-related postpartum hemorrhage, wherein bleeding persists despite the uterus exhibiting good tone, with a palpable firm uterine fundus.
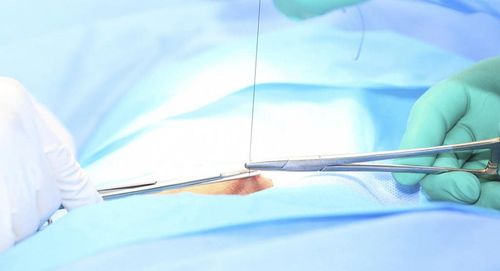
However, for a definitive diagnosis, a physician must conduct an examination utilizing a speculum to fully visualize the vaginal walls and cervix. Additionally, a heart-shaped clamp is employed to manipulate the cervical tissue in various directions to detect any injuries between the clamps. Local hemostasis should be performed to adequately observe and assess the characteristics of the laceration for timely and effective management.
If an actively bleeding laceration is observed or if bleeding has ceased, the patient requires local anesthesia for the surgical intervention, which entails suturing the laceration with absorbable sutures. This procedure necessitates the presence of an experienced obstetrician and one to two midwives to provide instrument assistance and support for the patient’s overall condition. In cases of significant bleeding due to complex cervical lacerations involving adjacent structures, if the patient exhibits signs of hypovolemic shock or hemorrhagic shock, immediate priority should be given to resuscitation, isotonic fluid replacement, and blood transfusion before proceeding to the surgical procedure in an operating room with complete monitoring and anesthesia-resuscitation support.
Post-procedure, the patient requires ongoing monitoring of vaginal bleeding and vital signs in either the delivery ward or recovery room until stability is achieved. If bleeding persists, re-evaluation is necessary, and additional suturing may be required. Monitoring blood loss volume, along with complete blood count, hemoglobin levels, and, if indicated, blood transfusion is essential. Furthermore, considering the risk of infection during procedural interventions, broad-spectrum intravenous antibiotics should be prescribed for five days, along with instructions for monitoring vaginal discharge post-discharge.
In summary, cervical laceration is a complication following vaginal delivery, particularly in cervices that have undergone prior interventions. Timely suturing of cervical lacerations is essential to minimize pain and blood loss for the patient. Nonetheless, preventive measures to avoid cervical lacerations should be prioritized, with instructions provided for safe vaginal delivery when conditions permit, and notably, the capability and experience to monitor the patient post-delivery to ensure a safe labor process.
To arrange an appointment, please call HOTLINE or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.